Larissa I. Velez
Most corrosive injuries involve acids or alkalis. Other corrosives damage tissues by various mechanisms, including oxidation, reduction, vesication, desiccation, metabolic inhibition, or cellular poisoning. Fluoride and hydrofluoric acid are discussed in Chapter 330, and chemical warfare agents (including the blistering agents) are discussed in Chapter 350. This chapter focuses on the damaging effects of acids and alkali.
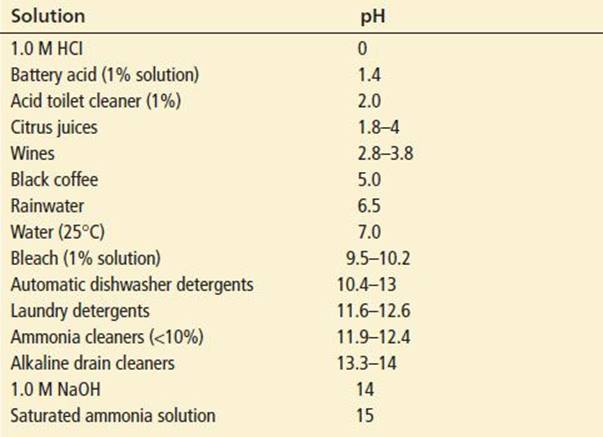
Acids (pH <7) are proton donors that dissociate into conjugate bases and free hydrogen ions (H+) in solution. Alkalis (pH >7) accept protons, resulting in the formation of conjugate acids and free hydroxide ions (OH−). In general, substances with a pH <3 or >11 have the most potential to cause significant corrosive injury, as they produce more free ions (Table 328.1). Acids denature proteins and cause coagulation necrosis. The formation of a firm coagulum or eschar often limits the penetration of injury. Alkalis cause liquefaction necrosis, which dissolves proteins and saponifies fats. The injured tissues slough, allowing for deeper injury when compared to acids.
TABLE 328.1
Approximate pH of Some Common Solutions
The extent, location, and severity of gastrointestinal (GI) injury depend on the physical state of the corrosive or chemical agent, the pH and concentration of the agent, the amount ingested, the duration of tissue contact, the presence of food in the stomach, and the tonicity of the pyloric sphincter. Solid particles dissolve on contact with body fluids, producing highly concentrated solutions, which may result in severe localized damage. Solids and viscous solutions tend to adhere to tissues and frequently result in proximal rather than distal involvement. Larger amounts, which are common with intentional ingestions, have a higher potential for severe injury. However, acids usually have a strong odor and result in immediate pain and smooth muscle spasm, which may limit the amount ingested. Alkalis are often odorless and do not cause immediate pain after contact. In addition, sloughing of tissue after liquefactive necrosis results in deeper penetration of alkalis. Because of these characteristics, alkali ingestions usually involve larger volumes and result in more severe injury. In general, longer contact times with a corrosive substance results in greater injury. Finally, the presence of food in the stomach is somewhat protective. Systemic toxicity sometimes accompanies severe GI injuries and is usually secondary to tissue inflammation, necrosis, perforation, acidosis, and infection. Fluid and electrolyte shifts can accompany extensive burns and result in hypovolemic shock. Some corrosives also cause systemic toxicity when absorbed.
The subsequent injury and repair processes are similar for both acids and alkali. There is bacterial invasion after 24 to 48 hours, an inflammatory response, and development of granulation tissue. Because collagen deposition may not begin until the second week, tensile strength of the healing tissue is low during the first 3 weeks (1). Scar retraction begins in the third week, commonly continuing for months, and may result in stricture formation. Finally, mucosal repair can take weeks to months.
Ocular damage is most severe following alkali burns as a result of early disruption of the corneal epithelium and rapid tissue penetration. As with ingestions, the overall severity of alkali burns is generally more than that seen with acids.
Chemical burns caused by corrosives differ in several important ways from thermal burns. First, the initial severity of the injury may be underestimated because tissue penetration of the chemical may be deeper than anticipated by visual inspection. In addition, tissue penetration and damage may continue for hours to days. Furthermore, absorption of the chemical may result in systemic toxicity. As with ingestions, the severity of the dermal injury is dependent on several factors, including the specific mechanism of toxicity and concentration of the agent, duration of exposure, surface area exposed, thickness of the skin involved, and depth of penetration. Patient factors such as age, pre-existing conditions of the skin, and concurrent illnesses also affect the severity of the injury.
CLINICAL PRESENTATION
Sites commonly affected by corrosive ingestion are the oropharynx, esophagus, and stomach, although injury may occur as far as the proximal jejunum (2,3). Injury to other organs, including the heart, liver, and pancreas, has been reported, but is rare (4,5).
Patients usually present with oral, throat, chest, or abdominal pain. Dysphagia, drooling, and vomiting are common. Children may refuse to drink, cry excessively, or be unable to swallow their secretions. Stridor, hoarseness, hematemesis, and melena occur less frequently (6). Tachypnea can occur from aspiration of the corrosive with resultant pneumonitis or as a compensation for a metabolic acidosis. The metabolic acidosis may reflect tissue necrosis or the systemic absorption of ingested acids.
On inspection, superficial burns of the oropharynx are often covered with a pale membrane, and deeper burns are black, hemorrhagic, or friable but the presence or absence of burns in the oropharynx does not reliably predict more distal injuries (3,6). Full-thickness injuries to the esophagus or stomach are at risk of perforation and fistula formation into the trachea, mediastinum, or peritoneum (3). Mediastinitis can present with chest pain, respiratory distress, fever, subcutaneous emphysema, pleural rub, and Hamman sign (an audible crunch with each heart beat). Chest radiographic findings of mediastinitis may include mediastinal widening, pleural effusion (usually left-sided), pneumomediastinum, and pneumothorax.
The abdominal examination is an unreliable indicator of the severity of the injury, but frank peritonitis is an ominous sign. Peritonitis may result from viscous perforation or the extension of severe gastric burns to surrounding abdominal organs. Patients with peritonitis may have marked third-spacing of fluids, resulting in abdominal distention and hypotension. Abdominal compartment syndrome, or intra-abdominal hypertension, has been reported.
The late presentations after a corrosive ingestion include dysphagia, nausea, and vomiting as a result of the formation of strictures. Esophageal strictures develop in up to 70% of patients with deep esophageal ulcers and in nearly all patients with areas of necrosis (3). Ulceration superficial to the muscularis mucosa layer does not lead to stricture formation. Half of all esophageal strictures develop during the initial hospitalization, and 80% are evident within 2 months. Esophageal carcinoma, a late sequela of alkali ingestion, has been diagnosed after a latency period of about 40 years (1) but is only rarely reported with acid burns.
Ocular injury most commonly results from splash exposures at home or in the work environment. Injuries have also been reported after airbag deployment, where sodium hydroxide is produced (7,8). The severity of these injuries ranges from transient irritation to severe disabling ocular damage and blindness. Manifestations include immediate eye pain, photophobia, blepharospasm, lacrimation, conjunctival injection or hemorrhage, and decreased visual acuity. The pupils may be nonreactive as a result of severe iritis. Intraocular pressure rises with damage to the trabecular meshwork, resulting in new glaucoma. With more significant involvement, chemosis and corneal edema, opacification, sloughing, ulceration, and necrosis occur. Destruction of blood vessels may result in a very white sclera indicative of corneal ischemia which along with corneal opacification are both ominous signs. If penetration is deep enough, retinal damage occurs. Ultimately, inflammation leads to fibrosis, synechiae, and cataract formation.
Dermal exposure usually results in immediate pain at the affected site, but the onset of pain can sometimes be delayed for several hours, especially with hydrofluoric acid (see Chapter 330). Petroleum distillates, weak sodium hydroxide solutions, and wet cement, which is an alkali, typically do not produce burns unless allowed to remain in contact with the skin for prolonged periods. Such exposures may initially appear trivial but can progress to full-thickness burns. Chemical burns rarely blister, and the affected skin is usually dark, insensate, and firmly attached regardless of the burn depth. With time, the skin hardens and cracks, exposing the underlying dermis or subcutaneous tissue. Healing of chemical burns usually takes longer than for thermal burns.
DIFFERENTIAL DIAGNOSIS
With ingestions, it is important to determine the coingestion of other agents. If shock or altered mental status is present soon after ingestion, other causes than caustics should be sought. The ingestion of heavy metals and hydrocarbons can cause symptoms similar to a caustic ingestion. Allergic reactions may also present with some of the features of corrosive ingestion, specifically if the hypopharynx or larynx is involved. Infections such as epiglottitis, croup, retropharyngeal abscess, and mucosal ulceration as a result of herpesvirus or coxsackievirus should be considered in children.
The differential diagnosis of corrosive injury to the eye includes traumatic corneal abrasion or ulceration, corneal foreign bodies, allergic reactions, infectious processes such as viral or bacterial conjunctivitis, iritis, iridocyclitis, acute narrow-angle glaucoma, and exposure to fumes, vapors, and other sensitizing agents.
Considerations in the differential diagnosis of chemical dermal injuries include thermal burns, radiation burns (including sunburns and from welding), mechanical irritation or trauma, allergic reactions and drug eruptions (such as Stevens–Johnson syndrome or toxic epidermal necrolysis), contact dermatitis, infections, and bacterial toxin-mediated conditions such as staphylococcal scalded skin syndrome or toxic shock syndrome.
ED EVALUATION
The identity, concentration, and amount of chemical or product involved and the time and circumstances of exposure should be determined as soon as feasible. Product labels, when available, should be examined for ingredients and signal words. The signal words “caution,” “warning,” and “danger” identify a product as a weak irritant (to eyes, nose, and throat), strong irritant (to skin and mucous membranes), or corrosive (capable of causing permanent or fatal tissue damage), respectively. If a sample is available, measure its pH. A pH meter is more accurate than pH paper (e.g., pHydrion paper, which is also used for testing amniotic fluid) but is not generally available. A regional poison-control center can assist with identifying the product and for advice on evaluation and management of the exposure. However, none of these should delay the patient evaluation and management.
In patients with corrosive ingestion, attention should initially be directed to airway patency, because obstruction may develop with progressive mucosal edema. In the absence of stridor or respiratory distress indicating the need for immediate endotracheal intubation, patients with a hoarse voice or respiratory symptoms should have the upper airway assessed by direct fiberoptic laryngoscopy. Patients suspected of having a significant corrosive injury should also have an electrocardiogram, blood-gas analysis, complete blood count, type and crossmatch, prothrombin time, electrolyte, glucose, liver-function, and renal-function tests. Radiologic studies should include an upright chest radiograph if the patient has respiratory symptoms and abdominal films if perforation is suspected.
Endoscopy of the upper GI tract is the gold standard for the diagnosis of corrosive injury (9). Endoscopy should be performed in all symptomatic patients. A complete lack of symptoms or signs suggests that significant injuries are absent and that endoscopy is not necessary (6). Nevertheless, endoscopy should be considered for asymptomatic patients who have intentionally ingested a strong acid or alkali or if the history is unreliable. Endoscopy is optimally performed 12 to 24 hours after exposure (3). If undertaken earlier, the full extent of injury may not be apparent; if performed later, the risk of perforation may be increased (2).
Esophageal and gastric burns are graded in a similar fashion as dermal burns. Grade 1 burns just have erythema of the mucosa (3). Grade 2 burns have partial-thickness submucosal lesions, ulceration, and exudates. Some authors consider 2 a burns as noncircumferential, and 2b as near circumferential. Grade 3 burns are deep, full-thickness burns with ulcers and necrosis into the periesophageal tissues (6). Third-degree burns have an 85% incidence of stricture development. Overall, the best predictor for the development of strictures is the severity of the initial injury. Endoscopic ultrasound has been used to measure injury to the muscularis layer. Injury to the muscularis layer has also been shown to correlate with late stricture formation (10). Contrast esophagography is less sensitive than endoscopy in assessing burn injury, although it is useful for detecting perforation. A water-soluble contrast agent (gastrografin) must be used whenever perforation is suspected. Cine-esophagogram can detect esophageal motility disorders and gastroesophageal reflux, which also predict stricture formation. CT scan has also been used for detection of stomach perforation. A grading scale for caustic burns on CT scan can be used (10).
With symptomatic ocular exposures, decontamination must always precede the formal evaluation of the eye. A complete eye examination including measurement of visual acuity, conjunctival pH, and a slit-lamp examination should follow the decontamination. If injury to the anterior chamber is suspected, the intraocular pressure should be measured. However, this last step must be avoided if there is a concern for ocular globe disruption.
The assessment of dermal injuries is similar to that for thermal burns. Location, size, color, texture, and neurovascular status should be noted. If the affected area is >5% of total body surface area or if systemic toxicity is possible, a more thorough physical examination and laboratory testing can be performed to assess for systemic involvement.
KEY TESTING
• Early endoscopy for all symptomatic caustic ingestions, regardless of oral findings
• Direct fiberoptic laryngoscopy for hoarseness, stridor, or respiratory symptoms
• Chest and abdominal radiographs, and esophagogram with low–molecular-weight contrast, for possible esophageal or gastric perforation
• Laboratories for supportive care include CBC, chemistries, and coagulation studies
• Conjunctival pH testing after eye irrigation
ED MANAGEMENT
Any patient with evidence of significant upper airway obstruction such as severe respiratory distress, stridor, or inability to speak should undergo immediate endotracheal intubation. Delay in securing a definitive airway will only result in further development of airway edema and increase the difficulty with endotracheal intubation. This, however, is a rare event (10).
The efficacy of GI decontamination is limited. However, the mouth should be rinsed liberally with water in patients with oral burns. Because emesis re-exposes the esophagus to the corrosive agent and increases the risk of aspiration, antiemetics should be given to patients with persistent nausea or vomiting. A nasogastric tube for stomach emptying may be considered in recent, large-volume ingestions. Activated charcoal should be avoided since it obscures the endoscopist’s view, and most corrosives are not significantly adsorbed by charcoal. Dilution of gastric contents with oral fluids within minutes of ingestion may be beneficial, although the current evidence is inconclusive (10). If dilution is to be used, it should be within minutes of exposure in patients with a normal airway and mental status, without significant nausea, vomiting, or pain, and who are able to speak and cooperate. The amount swallowed should be limited to 5 mL/kg to avoid inducing emesis.
Although corticosteroids reduce the incidence and severity of esophageal strictures in animal studies, their value in humans is controversial. In human trials in which steroids were not given until up to 24 hours after exposure, there are conflicting conclusions as well as points of general agreement. Patients with first-degree esophageal burns do not require steroids, because strictures do not develop in this group. Steroids do not appear to alter the development of esophageal strictures in patients with extensive areas of deep ulceration or necrosis (grade 3 burns) and may actually increase the rate of complications such as infection, hemorrhage, or perforation. For patients between these two extremes, whose injuries consist of circumferential or extensive superficial ulceration or small areas of deep ulceration or necrosis, steroids are of potential benefit. The most recent pooled analysis of the available data did not show a statistically significant benefit of steroids for second-degree burns (11). An earlier systematic review of published cases also failed to show benefit in second-degree burns (12). The decision to use steroids is based on the grading of the burns, which highlights the importance of early endoscopic evaluation.
Concomitant penicillin, ampicillin, or clindamycin are recommended whenever steroids are being used. Although they are of no proven benefit in promoting healing or reducing complications, antacids, sucralfate, H2 blockers, proton pump inhibitors, and analgesics (ibuprofen) can provide symptomatic relief (2,10). Oral medications and feedings should be withheld until after endoscopy, and then should be given only to patients with injuries limited to mucosal inflammation or small areas of superficial ulceration. These patients may be given oral fluids when they are able to swallow their own secretions. Those patients with more severe injuries should receive intravenous fluids and nothing by mouth.
Surgical exploration is indicated if perforation is confirmed by radiographs or endoscopy, when there is persistent hypotension, or in the presence of abdominal rigidity. Surgical exploration has also been recommended in patients who are at high risk of perforation, sepsis, necrosis, or hemorrhage. Because endoscopy cannot fully evaluate the depth of the burns (e.g., the status of the serosal surface), exploration has also been proposed for patients with grade 2 or 3 burns to overcome this limitation. In one study, a serum pH <7.22 and a base excess more than –12.0 were predictors of severe injury requiring an emergency salvage operation (10).
Immediate copious irrigation is the single most important intervention in the management of eye exposures (13). The severity of ocular damage at the time of presentation is a good predictor of the ultimate outcome, as are timeliness and adequacy of irrigation. Ideally, irrigation will have been performed immediately at the time of exposure in the home or workplace and continued en route to the hospital. The patient can use a running faucet or hold his or her breath while blinking while the face is in a pan of water. If the patient has significant pain, irrigation must again be performed in the emergency department (ED). Acceptable irrigation solutions include tap water, normal saline, Ringer lactate, or D5W. Commercially available irrigation solutions (Previn, Diphoterine) are also acceptable, but the irrigation should not be delayed while these solutions are obtained irrigation will be aided greatly with topical anesthetic solution, eyelid retractors, intravenous analgesics, or sedatives. The eyelids should be everted, and any particulate matter should be removed with a cotton swab. Continuous irrigation of the eye is made easier with use of a scleral lens with inflow channel (Morgan Therapeutic Lens), or one can simply irrigate manually with intravenous tubing connected to irrigation solution. Initially the eye should be irrigated with 1 L and for at least 20 minutes. For highly corrosive substances, especially alkali exposures, irrigation should continue for at least an hour.
After irrigation, the pH of the inferior cul-de-sac should be tested with litmus or pH paper. If a neutral pH of 7 to 8 has not yet been achieved, continued irrigation is warranted. Once a neutral conjunctival pH is achieved, the pH should be rechecked every 30 minutes for 2 hours, because corrosive material may be slowly released from corneal tissue for several hours. A subsequent change in pH indicates the need for further irrigation.
Standard treatment for corneal injuries includes topical antibiotics, steroids, cycloplegics, and mydriatics. If intraocular pressure is elevated, topical timolol maleate and oral acetazolamide may be required. Tetanus prophylaxis and analgesics should be administered if needed.
Initial management of dermal injuries is also directed at rapid decontamination with copious water irrigation of the skin surface with water for most exposures. Ideally, irrigation will have been initiated immediately at the scene and continued en route to the hospital (14). Delayed decontamination can result in increased tissue damage and deeper penetration of the offending agent. In industrial accidents, rescuers should wear appropriate protective gear such as gloves, gowns, masks, and eye shields. All contaminated clothing, footwear, jewelry, and contact lenses should be removed from the victim. Immediate irrigation with water should never be delayed to search for an alternative irrigation solution. Irrigation should continue for at least 20 minutes. A longer period of irrigation lasting up to several hours is required for alkalis and other serious exposures. Gently brush away particulate material before irrigation is started. Adherent materials may be removed by gentle scrubbing with soapy water while avoiding abrasions. Appropriate analgesia and tetanus prophylaxis should be provided, and wounds should be treated with topical antibiotic cream and protective dressings.
Irrigation should not be performed for burns caused by elemental forms of alkali metals such as sodium, potassium, lithium, cesium, and rubidium. These elements react with water to form hydroxides, strong bases that will significantly increase tissue damage. Furthermore, ignition or explosion occurs when water contacts pure magnesium, sulfur, strontium, titanium, uranium, yttrium, zinc, and zirconium. These two groups of substances should be covered with mineral oil to isolate them from water. Any solid particles that are removed from the victim must be stored in mineral oil to prevent further reactivity. These specific caustic agents are not commonly available and are thus seldom encountered. Patients with such exposures may come to the ED with Material Safety Data Sheets (MSDS) from their workplace. These data sheets can provide specific information about the agent.
CRITICAL INTERVENTIONS
• Evaluate the airway in patients with ingestions or facial-skin exposures, and intubate patients with respiratory distress, stridor, or inability to speak.
• Begin irrigation immediately, and continue for at least 20 minutes in symptomatic patients with eye and skin exposures.
• Consult a gastroenterologist for the endoscopy of patients with GI symptoms or suicidal corrosive ingestion.
• Consult a surgeon for patients with evidence of perforation, endoscopic evidence of severe GI injury, peritoneal signs, hypotension, or metabolic acidosis after corrosive ingestion.
• Consult an ophthalmologist for patients who have evidence of corneal injury or persistent pain after eye exposure.
• Consult a regional burn center for patients with significant dermal injury.
DISPOSITION
Exposed patients who are asymptomatic or become asymptomatic after oral rinsing and dilution may be discharged from the ED after an observation period (1). It is generally agreed that patients who are asymptomatic after unintentional ingestions will have normal endoscopies (6). For patients with more significant exposures, endoscopy should be arranged, with transfer to an appropriate facility if necessary. Suspected suicidal ingestions should have a psychiatric evaluation and the possibility of nonaccidental injury should be considered in all pediatric cases (1). Patients with no visible injury on endoscopy and those with injuries limited to mucosal inflammation or small areas of superficial ulceration may be medically discharged as long as they are able to tolerate oral fluids (15). Patients with persistent symptoms or inconclusive findings at endoscopy should be admitted for observation. If symptoms persist, endoscopy should be repeated.
Patients with mild chemical conjunctivitis can be referred to an ophthalmologist for follow-up the next day. Immediate ophthalmology consultation should be obtained for those with evidence of corneal injury or persistent pain. Patients with significant eye injuries should be admitted to the hospital for further irrigation, for assessment of injury progression and the need for surgical intervention, and to ensure initial compliance with the medical regimen.
Consultation with a general surgeon, plastic surgeon, or regional burn center is recommended for patients with significant dermal injuries. Patients with minor injuries may be discharged, if the patient is reliable and follow-up the next day can be arranged. Patients with systemic toxicity; second- or third-degree burns; extensive first-degree burns (>5% of body surface area); burns to the face, eyes, ears, perineum, hands and feet; and high-risk patients such as those with significant pre-existing illness, the elderly, and psychiatric or otherwise noncompliant patients should be admitted (16).
Common Pitfalls
• Inducing vomiting by giving excessive amounts of oral fluid for dilution.
• Giving activated charcoal, which is not indicated for acid or alkali ingestion, and which will obscure endoscopic evaluation.
• Assuming that the absence of oropharyngeal burns precludes the presence of significant GI injury in symptomatic patients.
• Failing to continue eye irrigation long enough, as determined by conjunctival pH testing.
• Underestimating the severity of dermal exposures and failing to provide adequate decontamination.
ACKNOWLEDGMENT
The author acknowledges the contributions of Collin S. Goto in previous editions of this chapter.
REFERENCES
1. Wilsey MJ Jr, Scheimann AO, Gilger MA. The role of upper gastrointestinal endoscopy in the diagnosis and treatment of caustic ingestion, esophageal strictures, and achalasia in children. Gastrointest Endosc Clin N Am.2001;11(4):767–787, vii–viii.
2. de Jong AL, Macdonald R, Ein S, et al. Corrosive esophagitis in children: A 30-year review. Int J Pediatr Otorhinolaryngol. 2001;57(3):203–211.
3. Zargar SA, Kochhar R, Mehta S, et al. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc. 1991;37(2):165–169.
4. Aggarwal A, Bansal A, Dixit A, et al. Heartburn literally: Cardiac injury due to corrosive ingestion. J Postgrad Med. 2013;59(2):152–153.
5. Nijhawan S, Jain P. Acute pancreatitis as an unusual complication of corrosive ingestion. J Gastrointestin Liver Dis. 2007;16(3):345–346.
6. Gorman RL, Khin-Maung-Gyi MT, Klein-Schwartz W, et al. Initial symptoms as predictors of esophageal injury in alkaline corrosive ingestions. Am J Emerg Med. 1992;10(3):189–194.
7. Barnes SS, Wong W Jr, Affeldt JC. A case of severe airbag related ocular alkali injury. Hawaii J Med Public Health. 2012;71(8):229–231.
8. Corazza M, Trincone S, Virgili A. Virgili, Effects of airbag deployment: Lesions, epidemiology, and management. Am J Clin Dermatol. 2004;5(5):295–300.
9. Rigo GP, Camellini L, Azzolini F, et al. What is the utility of selected clinical and endoscopic parameters in predicting the risk of death after caustic ingestion? Endoscopy. 2002;34(4):304–310.
10. Contini S, Scarpignato C.Caustic injury of the upper gastrointestinal tract: A comprehensive review. World J Gastroenterol. 2013;19(25):3918–3930.
11. Fulton JA, Hoffman RS. Steroids in second degree caustic burns of the esophagus: A systematic pooled analysis of fifty years of human data: 1956–2006. Clin Toxicol (Phila). 2007;45(4):402–408.
12. Pelclová D, Navrátil T. Do corticosteroids prevent oesophageal stricture after corrosive ingestion? Toxicol Rev. 2005;24(2):125–129.
13. Saidinejad M, Burns MM. Ocular irrigant alternatives in pediatric emergency medicine. Pediatr Emerg Care. 2005;21(1):23–26.
14. Leonard LG, Scheulen JJ, Munster AM. Chemical burns: Effect of prompt first aid. J Trauma. 1982;22(5):420–423.
15. Estrera A, Taylor W, Mills LJ, et al. Corrosive burns of the esophagus and stomach: A recommendation for an aggressive surgical approach. Ann Thorac Surg. 1986;41(3):276–283.
16. Fitzpatrick KT, Moylan JA. Emergency care of chemical burns. Postgrad Med. 1985;78(5):189–194.