Definition
Chronic elevation in bp (systolic ≥140 mmHg or diastolic ≥90 mmHg); etiology unknown in 80–95% of pts (“essential hypertension”). Always consider a secondary correctable form of hypertension, especially in pts under age 30 or those who become hypertensive after 55. Isolated systolic hypertension (systolic ≥140, diastolic <90) most common in elderly pts, due to reduced vascular compliance.
SECONDARY HYPERTENSION
Renal Artery Stenosis (Renovascular Hypertension)
Due to either atherosclerosis (older men) or fibromuscular dysplasia (young women). Presents with recent onset of hypertension, refractory to usual antihypertensive therapy. Abdominal bruit is present in 50% of cases; often audible; mild hypokalemia due to activation of the renin-angiotensinaldosterone system may be present.
Renal Parenchymal Disease
Elevated serum creatinine and/or abnormal urinalysis, containing protein, cells, or casts.
Coarctation of Aorta
Presents in children or young adults; constriction is usually present in aorta at origin of left subclavian artery. Exam shows diminished, delayed femoral pulsations; late systolic murmur loudest over the midback. CXR shows indentation of the aorta at the level of the coarctation and rib notching (due to development of collateral arterial flow).
Pheochromocytoma
A catecholamine-secreting tumor, typically of the adrenal medulla or extraadrenal paraganglion tissue, that presents as paroxysmal or sustained hypertension in young to middle-aged pts. Sudden episodes of headache, palpitations, and profuse diaphoresis are common. Associated findings include chronic weight loss, orthostatic hypotension, and impaired glucose tolerance. Pheochromocytomas may be localized to the bladder wall and may present with micturition-associated symptoms of catecholamine excess. Diagnosis is suggested by elevated plasma metanephrine level or urinary catecholamine metabolites in a 24-h urine collection (see below); the tumor is then localized by CT scan or MRI.
Hyperaldosteronism
Usually due to aldosterone-secreting adenoma or bilateral adrenal hyper-plasia. Should be suspected when hypokalemia is present in a hypertensive pt off diuretics (Chap. 182).
Other Causes
Oral contraceptive usage, obstructive sleep apnea (Chap. 146), Cushing’s and adrenogenital syndromes (Chap. 182), thyroid disease (Chap. 181), hyperparathyroidism, and acromegaly (Chap. 179). In pts with systolic hypertension and wide pulse pressure, consider thyrotoxicosis, aortic regurgitation (Chap. 123), and systemic AV fistula.
APPROACH TO THE PATIENT Hypertension
History: Most pts are asymptomatic. Severe hypertension may lead to headache, dizziness, or blurred vision.
Clues to specific forms of secondary hypertension: Use of medications (e.g., birth control pills, glucocorticoids, decongestants, erythropoietin, NSAIDs, cyclosporine); paroxysms of headache, sweating, or tachycardia (pheochromocytoma); history of renal disease or abdominal trauma (renal hypertension); daytime somnolence and snoring (sleep apnea).
Physical examination: Measure bp with appropriate-sized cuff (large cuff for large arm). Measure bp in both arms as well as a leg (to evaluate for aortic coarctation). Signs of hypertension include retinal arteriolar changes (narrowing/nicking); left ventricular lift, loud A2, S4. Clues to secondary forms of hypertension include cushingoid appearance, thyro-megaly, abdominal bruit (renal artery stenosis), delayed femoral pulses (coarctation of aorta).
Laboratory Workup
Screening tests for secondary hypertension: Should be carried out on all pts with documented hypertension: (1) serum creatinine, BUN, and urinalysis (renal parenchymal disease); (2) serum K measured off diuretics (hypokalemia prompts workup for hyperaldosteronism or renal artery stenosis); (3) CXR (rib notching or indentation of distal aortic arch in coarctation of the aorta); (4) ECG (LV hypertrophy suggests chronicity of hypertension); (5) other useful screening blood tests including CBC, glucose, lipid levels, calcium, uric acid; (6) thyroid-stimulating hormone if thyroid disease suspected.
Further workup: Indicated for specific diagnoses if screening tests are abnormal or bp is refractory to antihypertensive therapy: (1) renal artery stenosis: magnetic resonance angiography, captopril renogram, renal duplex ultrasound, digital subtraction angiography, renal arteriography; (2) Cushing’s syndrome: dexamethasone suppression test (Chap. 182); (3) pheochromocytoma: 24-h urine collection for catecholamines, meta-nephrines, and vanillylmandelic acid and/or measurement of plasma metanephrine; (4) primary hyperaldosteronism: depressed plasma renin activity and hypersecretion of aldosterone, both of which fail to change with volume expansion; (5) renal parenchymal disease (Chap. 149).
TREATMENT Hypertension
Helpful lifestyle modifications include weight reduction (to attain BMI <25 kg/m2); sodium restriction; diet rich in fruits, vegetables, and low-fat dairy products; regular exercise; and moderation of alcohol consumption.
DRUG THERAPY OF ESSENTIAL HYPERTENSION (SEE TABLE 126-1 AND FIG. 126-1) Goal is to control hypertension with minimal side effects. A combination of medications with complementary actions is often required. First-line agents include diuretics, ACE inhibitors, angiotensin receptor antagonists, calcium channel antagonists, and beta blockers. On-treatment blood pressure goal is <135–140 systolic, <80–85 diastolic (<130/80 in pts with diabetes or chronic kidney disease).
TABLE 126-1 ORAL DRUGS COMMONLY USED IN TREATMENT OF HYPERTENSION
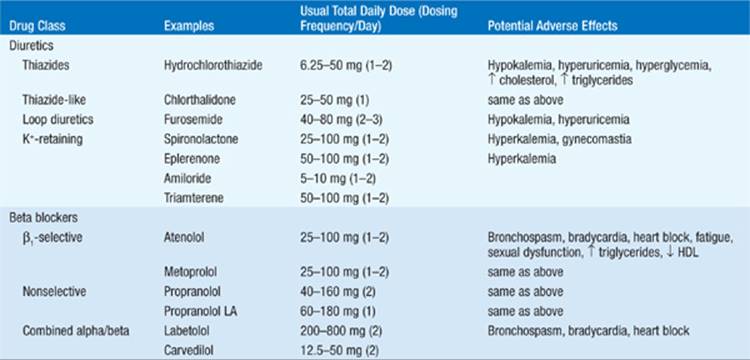
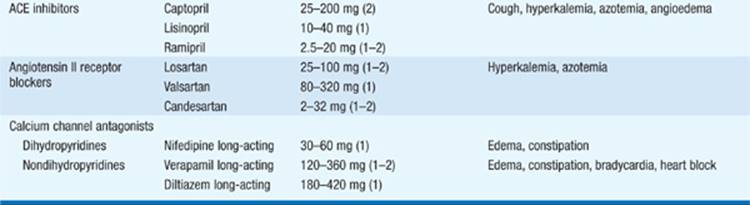
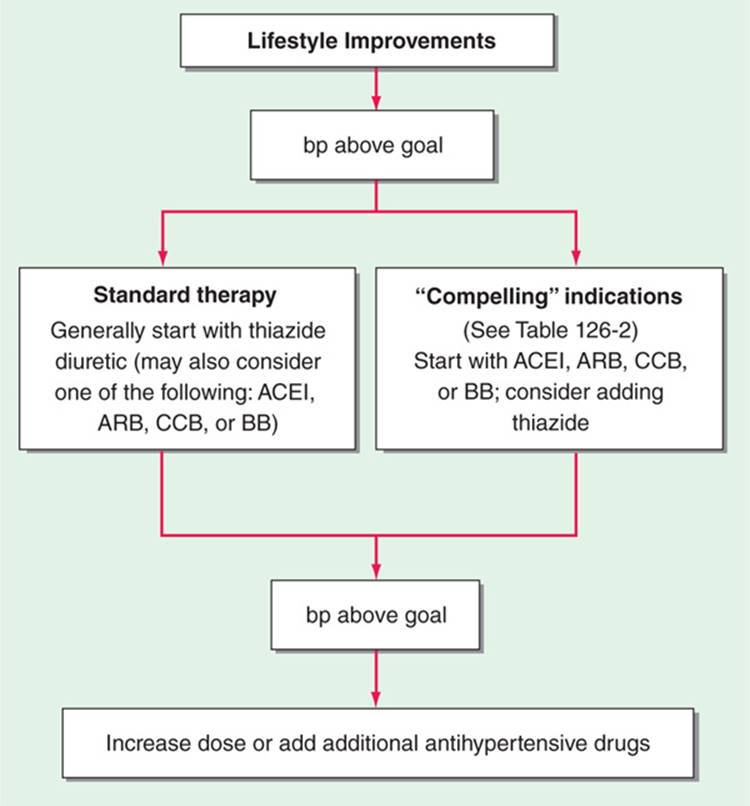
FIGURE 126-1 Initiation of therapy in pts with hypertension. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; BB, beta blocker.
Diuretics Should be cornerstone of most antihypertensive regimes. Thiazides preferred over loop diuretics because of longer duration of action; however, the latter are more potent when serum creatinine >2.5 mg/dL. Major side effects include hypokalemia, hyperglycemia, and hyperuricemia, which can be minimized by using low dosage (e.g., hydrochlorothiazide 6.25–50 mg qd). Diuretics are particularly effective in elderly and black pts. Prevention of hypokalemia is especially important in pts on digitalis glycosides.
ACE Inhibitors and Angiotensin II Receptor Blockers (ARBs) ACE inhibitors and ARBs are well tolerated with low frequency of side effects. May be used as monotherapy or in combination with a diuretic, calcium antagonist, or beta blocker. Side effects are uncommon and include angioedema (more common with ACE inhibitors than ARBs), hyperkalemia, and azotemia (particularly in pts with elevated baseline serum creatinine). A nonproductive cough may develop in the course of therapy in up to 15% of pts on an ACE inhibitor, prompting substitution with an ARB (cough is not common side effect) or alternate antihypertensives. Note that renal function may deteriorate rapidly as a result of inhibition of the renin-angiotensin system in pts with bilateral renal artery stenosis.
Potassium supplements and potassium-sparing diuretics should be used cautiously with ACE inhibitors or ARBs to prevent hyperkalemia. If pt is intravascularly volume depleted, hold diuretics for 2–3 days prior to initiation of drug, which should then be administered at low dosage.
Calcium Antagonists Direct arteriolar vasodilators; all have negative inotropic effects (particularly verapamil) and should be used cautiously if LV dysfunction is present. Verapamil and, to a lesser extent, diltiazem can result in bradycardia and AV block, so combination with beta blockers is generally avoided. Use sustained-release formulations, as short-acting dihydropyridine calcium channel blockers may increase incidence of coronary events. Common side effects include peripheral edema and constipation.
If bp proves refractory to drug therapy, work up for secondary forms of hypertension, especially renal artery stenosis and pheochromocytoma. Beta Blockers Particularly useful in young pts with “hyperkinetic” circulation. Begin with low dosage (e.g., metoprolol succinate 25–50 mg daily). Relative contraindications: bronchospasm, CHF, AV block, bradycardia, and “brittle” insulin-dependent diabetes.
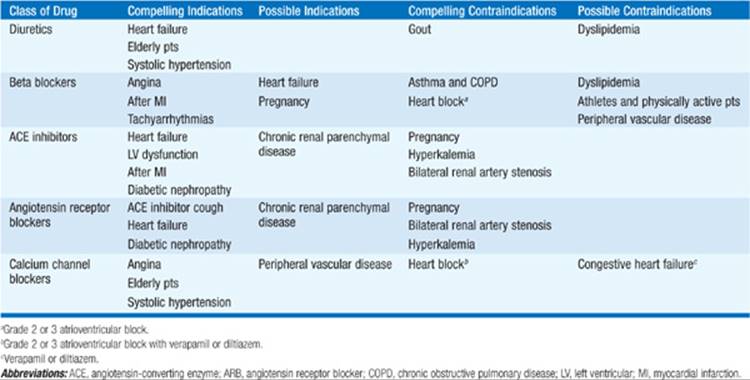
Table 126-2 lists compelling indications for specific initial drug treatment.
TABLE 126-2 GUIDELINES FOR SELECTING INITIAL DRUG TREATMENT OF HYPERTENSION a
SPECIAL CIRCUMSTANCES
Pregnancy Most commonly used antihypertensives include methyldopa (250–1000 mg PO bid-tid), labetalol (100–200 mg bid), and hydralazine (10–150 mg PO bid-tid). Calcium channel blockers (e.g., nifedipine, long-acting, 30–60 mg daily) also appear to be safe in pregnancy. Beta blockers should be used cautiously; fetal hypoglycemia and low birth weights have been reported. ACE inhibitors and ARBs are contraindicated in pregnancy.
Renal Disease Standard thiazide diuretics may not be effective. Consider metolazone, furosemide, or bumetanide, alone or in combination.
Diabetes Goal bp <130/80. Consider ACE inhibitors and angiotensin receptor blockers as first-line therapy to control bp and slow renal deterioration.
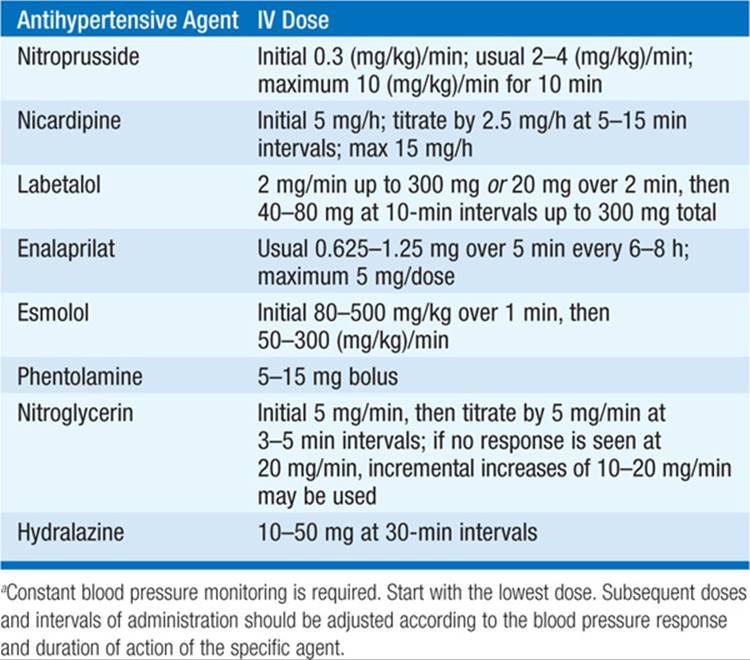
Malignant Hypertension Defined as an abrupt increase in bp in pt with chronic hypertension or sudden onset of severe hypertension; a medical emergency. Immediate therapy is mandatory if there is evidence of cardiac decompensation (CHF, angina), encephalopathy (headache, seizures, visual disturbances), or deteriorating renal function. Inquire about use of cocaine, amphetamines, or monoamine oxidase inhibitors. Drugs to treat hypertensive crisis are listed in Table 126-3. Replace with PO antihypertensive as pt becomes asymptomatic and bp improves.
TABLE 126-3 USUAL INTRAVENOUS DOSES OF ANTIHYPERTENSIVE AGENTS USED IN HYPERTENSIVE EMERGENCIESa

For a more detailed discussion, see Kotchen TA: Hypertensive Vascular Disease, Chap. 247, p. 2042, in HPIM-18.