The neurohypophysis, or posterior pituitary gland, produces two hormones: (1) arginine vasopressin (AVP), also known as antidiuretic hormone (ADH), and (2) oxytocin. AVP acts on the renal tubules to induce water retention, leading to concentration of the urine. Oxytocin stimulates post-partum milk letdown in response to suckling. Its physiologic role in parturition is not established. Clinical syndromes may result from deficiency or excess of AVP.
DIABETES INSIPIDUS
Etiology
Diabetes insipidus (DI) results from insufficient AVP production by the hypothalamus or from impaired AVP action in the kidney. AVP deficiency is characterized by production of large amounts of dilute urine. In central DI, insufficient AVP is released in response to physiologic stimuli. Causes include acquired (head trauma; neoplastic or inflammatory conditions affecting the hypothalamus/posterior pituitary), congenital, and genetic disorders, but almost half of cases are idiopathic. In gestational DI, increased metabolism of plasma AVP by an aminopeptidase (vasopressinase) produced by the placenta leads to a relative deficiency of AVP during pregnancy. Primary polydipsiaresults in secondary insufficiency of AVP due to physiologic inhibition of AVP secretion by excessive fluid intake. Nephrogenic DIis caused by AVP resistance in the kidney; it can be genetic or acquired from drug exposure (lithium, demeclocycline, amphotericin B), metabolic conditions (hypercalcemia, hypokalemia), or renal damage.
Clinical Features
Symptoms include polyuria, excessive thirst, and polydipsia, with a 24-h urine output of >50 mL/kg/day and a urine osmolality that is less than that of serum (<300 mosmol/kg; specific gravity <1.010). DI can be partial or complete; in the latter case the urine is maximally diluted (<100 mosmol/kg) and the daily urine output can reach 10–20 L. Clinical or laboratory signs of dehydration, including hypernatremia, occur only if the pt simultaneously has a thirst defect (not uncommon in pts with CNS disease) or does not have access to water. Other etiologies of hypernatremia are described in Chap. 2.
Diagnosis
DI must be differentiated from other etiologies of polyuria (Chap. 52). Unless an inappropriately dilute urine is present in the setting of serum hyperosmolality, a fluid deprivation test is used to make the diagnosis of DI. This test should be started in the morning, and body weight, plasma osmolality, serum sodium, and urine volume and osmolality should be measured hourly. The test should be stopped when body weight decreases by 5% or plasma osmolality/sodium exceed the upper limit of normal. If the urine osmolality is <300 mosmol/kg with serum hyperosmolality, desmopressin (0.03 μg/kg SC) should be administered with repeat measurement of urine osmolality 1–2 h later. An increase of >50% indicates severe pituitary DI, whereas a smaller or absent response suggests nephrogenic DI. Measurement of AVP levels before and after fluid deprivation may be required to diagnose partial DI. Occasionally, hypertonic saline infusion may be required if fluid deprivation does not achieve the requisite level of hypertonic dehydration, but this should be administered with caution.
TREATMENT Diabetes Insipidus
Pituitary DI can be treated with desmopressin (DDAVP) subcutaneously (1–2 μg once or twice per day), via nasal spray (10–20 μg two or three times a day), or orally (100–400 μg two or three times a day), with recommendations to drink to thirst. Symptoms of nephrogenic DI may be ameliorated by treatment with a thiazide diuretic and/or amiloride in conjunction with a low-sodium diet, or with prostaglandin synthesis inhibitors (e.g., indomethacin).
SYNDROME OF INAPPROPRIATE ANTIDIURETIC HORMONE (SIADH)
Etiology
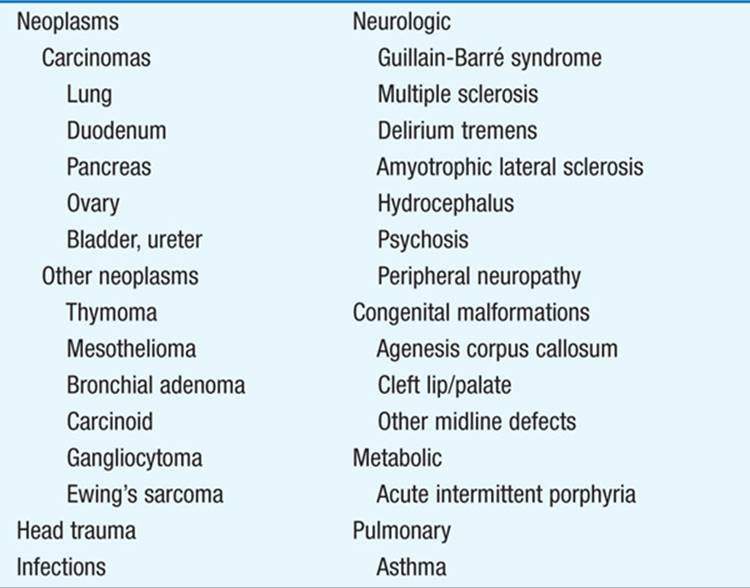
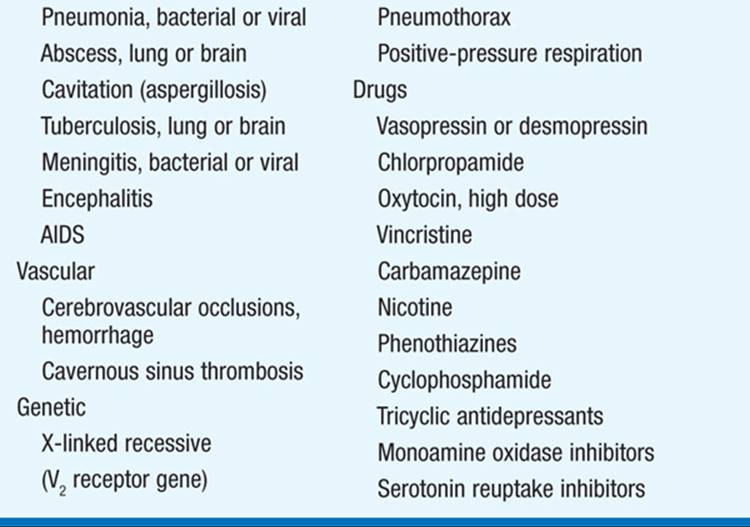
Excessive or inappropriate production of AVP predisposes to hyponatremia, reflecting water retention. The evaluation of hyponatremia is described in Chap. 2. Etiologies of SIADH include neoplasms, lung infections, CNS disorders, and drugs (Table 180-1).
TABLE 180-1 CAUSES OF SYNDROME OF INAPPROPRIATE ANTIDIURETIC HORMONE (SIADH)
Clinical Features
If hyponatremia develops gradually, it may be asymptomatic until it reaches a severe stage. However, if it develops acutely, symptoms of water intoxication may include mild headache, confusion, anorexia, nausea, vomiting, coma, and convulsions. Laboratory findings include low BUN, creatinine, uric acid, and albumin; serum ![]() meq/L and plasma osmolality <270 mosmol/kg; urine is not maximally diluted and frequently hypertonic to plasma, and urinary Na+ is usually >20 mmol/L.
meq/L and plasma osmolality <270 mosmol/kg; urine is not maximally diluted and frequently hypertonic to plasma, and urinary Na+ is usually >20 mmol/L.
TREATMENT SIADH
Fluid intake should be restricted to 500 mL less than urinary output. In pts with severe symptoms or signs, hypertonic (3%) saline can be infused at ≤0.05 mL/kg body weight IV per minute, with hourly sodium levels measured until Na increases by 12 meq/L or to 130 meq/L, whichever occurs first. However, if the hyponatremia has been present for >24–48 h and is corrected too rapidly, saline infusion has the potential to produce central pontine myelinolysis, a serious, potentially fatal neurologic complication caused by osmotic fluid shifts. Demeclocycline (150–300 mg PO three or four times a day) or fludrocortisone (0.05–0.2 mg PO twice a day) may be required to manage chronic SIADH. Vasopressin antagonists (conivaptan, tolvaptan) are available, but experience with these agents in SIADH treatment is limited.

For a more detailed discussion, see Robertson GL: Disorders of the Neurohypophysis, Chap. 340, p. 2902, in HPIM-18.