Etiology
• Most 2/2 ascending infxns; only ∼4% children w/ UTI/pyelonephritis are bacteremic
Microbiology
• 80% of infections 2/2 E. coli
• Gram-neg rods (Klebsiella, Proteus, Enterobacter, Citrobacter) = 2nd most common group
• Gram-pos cocci (Enterococcus, Staph. saprophyticus [mostly adol], Staph. aureus [rare])
• ↑ rates bacterial resistance in community acquired strains; risk for resistant infection inc w/prolonged or recent hospitalization, instrumentation, indwelling Foley
• Mediated by interaction of bacterial adhesins and receptors on host cells (e.g., E. coli pili – virulence factor → adhere to uroepithelium and ascend)
Risk Factors (Arch Dis Child 2006;91:845; Pediatrics 1998;102:e16)
• Age: Females <4 yo and males <1 yo
• FHx: Patients w/ 1° relatives w/ h/o childhood UTI more likely to have UTI (↑ adherence)
• Female (2/2 shorter urethra, possible ↑ adherence to female periurethral mucosa)
• Uncircumcised (mucosal foreskin vs. keratinized glans; partial phimosis → mild obstruction)
• Voiding dysfunction (frequent/infrequent voiding; urinary/stool incontinence; withholding); ∼15% prevalence in school-aged children
• Dx of exclusion after H&P/U/A/bladder U/S; often overlooked UTI risk-factor
• ∼40% school-aged pts w/ 1st UTI & 80% w/ recurrent UTI have sx c/w voiding dysfxn
• Risk factor for persistent vesicoureteral reflux (VUR) and renal scarring
• VUR; 2/2 short intravesical ureter > posterior urethral valves
• ∼1% prevalence in childhood; ∼40% of children w/ febrile UTIs; less common in AAs
• Grades I–V, depending on prox vs. distal reflux and presence/severity of ureteral
dilatation; ∼95% of VUR is Grades I–III
• Equivocal studies about link between VUR and pyelonephritis/renal scarring
• Most w/ recurrent pyelo or scarring do not have VUR
• Most VUR resolves w/i 5 yr
• Obstruction (anatomic [post urethral valves, UPJ obstruction, constipation] ∼1–4%; neurologic bladder; functional withholding)
• Sexual activity (strong correlation in sexually active adolescent and young adult females)
Clinical Manifestations
• Fever, abd or back pain, dysuria, ↑ urinary frequency, urgency or incontinence, hematuria, suprapubic tenderness (JAMA 2007;298:2895)
Diagnostic Studies (Pediatrics 2011;128:e749; Pediatr Infect Dis J 2002;21:1)
• Samples for UA and cx: Midstream clean catch if possible. Otherwise, cath or suprapubic
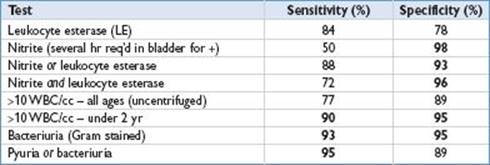
• “Enhanced U/A”; uncentrifuged U/A + GS + quantitative WBC/cc; most accurate screening test
• Difficult to distinguish cystitis from pyelonephritis via clinical criteria (some show pyelo on DMSA) → treat febrile UTI like pyelo in children <2 yo = 14 d Abx course
• Urine culture very important to guide management
• Cath urine cx significant if >1,000–50,000 CFU/mL especially if UA suggestive of an UTI if single pathogenic organism and consistent clinical picture
• Urine cx >50,000 CFU/mL indicator of significant bacteriuria if single pathogen present
• Clean-catch urine cx significant if >100,000 CFU/mL
• Up to 85% of +cx’s from bag urine specimens represent false-+ results
• Suprapubic bladder tap cx significant if any pathogenic bacteria present
• Blood cultures not routinely recommended in children >2 mo
• Need LP in children <1 mo, since 1% w/ UTI may have concurrent bacterial meningitis; LP for older infants is not absolutely indicated
• ↑ WBC, CRP not good predictors for UTI
• Pyuria present in UTI but not asymptomatic bacteriuria
• Consider checking serum creatinine if suspect acute renal failure 2/2 pyelonephritis
• Imaging: Renal U/S on all 1st UTIs (eval hydronephrosis) or pts w/ worsening dz (r/o abscess). Optimal imaging strategies controversial (Curr Opin Pediatr 2007;19:705)
• VCUG now only recommended if hydronephrosis, scarring, or anatomical abnormality found on renal ultrasound (Pediatrics 2011;128:e749)
• VCUG can be done as soon as cx negative (eval reflux, bladder anatomy, obstruction and voiding patterns) (Isr Med Assoc J 2008;10:453)
• Large prospective trial (RIVUR) study underway to evaluate role of antibiotic prophylaxis in children with VUR
• Antibiotic prophylaxis currently only recommended for patients with higher grade VUR (III–V), structural abnormalities, or urinary/bowel dysfunction
Management (Pediatrics 2011;128:e749; Pediatrics 2011;128:595; Pediatr Nephrol 2011;26:1967; N Engl J Med 2011;365:239; Pediatrics 2006;117:626; Pediatrics 2006;117:919; Arch Dis Child 2002;87:118)
• Base Rx on Ucx results & sensitivities or w/o these then local abx resistance patterns
• Initial antibiotic choice and route should be based on age of pt, clinical status, comorbidities, and associated problems (e.g., bacteremia)
• Empiric Rx in newborns & young infants: Amp + gent; to treat E.coli and E. faecilis
• Empiric Rx in ill appearing children: 3rd-gen cephalosporin (ceftriaxone, cefotaxime) and/or gentamicin (if possible bacteremia): Add amp if enterococcus suspected
• Most pts (infants >3 mo and children) are outpt Rx candidates (based on resistance): Amoxicillin; amoxicillin/clavulanate; TMP/SMX; cefixime; quinolones (effective, though safety concerns in younger children, now w/ FDA warning, risk of arthopathy)
• IV therapy for neonates/infants and children w/ urinary tract abnormalities/toxic/unable to PO/concern for noncompliance w/ treatment and follow-up
• Rx duration: For younger children typically 10–14 d w/ pyelonephritis (IV and PO) and 7 d for cystitis; 3 d for uncomplicated 1st UTI in older adolescents, males w/ UTI typically considered complicated (10–14 d Rx)
• Patients and families should be instructed to seek medical care with any recurrence of UTI symptoms after initial UTI diagnosis to prevent subsequent scarring