Daniel J. Deziel, M.D.
1 Which surgeon performed the world’s first known cholecystectomy?
A Karl Langenbuch
B Justus Ohage
C Hans Kehr
D Lawson Tait
E Eric Mühe
Ref.: 1
Comments
Karl Langenbuch performed the first operation to remove the gallbladder on July 15, 1882. Before that and, in fact, even for years afterward, patients with symptomatic gallstone disease were treated only with ineffective medical remedies or, occasionally, by cholecystostomy to drain the gallbladder. The first cholecystectomy in the Western Hemisphere was performed 4 years later by Justus Ohage in St. Paul, Minnesota. Hans Kehr of Halberstadt and Berlin was an early pioneer in biliary surgery. In 1901, he published a remarkable book describing more than 500 operations for gallstones, including 96 common bile duct operations. Kehr died of sepsis caused by a hand infection incurred after digital exploration of the common bile duct. Lawson Tait was a famed nineteenth-century English surgeon who advocated cholecystostomy rather than cholecystectomy. Eric Mühe performed the first “laparoscopic” cholecystectomy in Germany in 1985. Although technically different from modern laparoscopic cholecystectomy, it was a landmark contribution. Mühe was severely criticized and, in fact, vilified by the surgical community at the time. Only years later was the significance of his accomplishment recognized.
Answer
A
2 During palpation of the hepatoduodenal ligament, a pulsation is felt dorsal and slightly to the right of the common bile duct. Which of the following does this pulsation most likely represent?
A A normal common hepatic artery
B A normal right hepatic artery
C A replaced right hepatic artery
D A gastroduodenal artery
E A right renal artery
Ref.: 2, 3
Comments
The most common variation in hepatic arterial anatomy is origination of the right hepatic artery from the superior mesenteric artery. This is a replaced hepatic artery and not simply an accessory vessel that can be sacrificed with impunity. When an operation is performed in the right upper part of the abdomen, the pulsations encountered in the porta hepatis and gastrohepatic ligaments should be assessed. If the hepatic artery is absent or small, the surgeon must be alert to the possibility of a replaced hepatic vessel. When the right hepatic artery originates from the superior mesenteric artery, it courses dorsal to the head of the pancreas and the portal vein and is usually identified dorsolateral to the common bile duct. This vessel and its origin can readily be identified with intraoperative ultrasonography. Only rarely does a replaced right hepatic artery course through the pancreas. A replaced left hepatic artery originates from the left gastric artery and is located in the gastrohepatic ligament, where it is frequently encountered during operations on the stomach and gastroesophageal junction.
Answer
C
3 Which of the following an anatomic features may contribute to stricture formation after injury to the common bile duct?
A The blood supply to the supraduodenal bile duct has a longitudinal pattern.
B The blood supply to the supraduodenal bile duct has a lateral pattern.
C The blood supply to the supraduodenal bile duct has a segmental end-artery arrangement.
D The blood supply to the common bile duct is derived primarily from the common hepatic artery.
E The blood supply to the common bile duct has a fragile anastomotic network.
Ref.: 2-4
Comments
Ischemia is an important contributing factor to the development of postoperative bile duct stricture. The blood supply to the area of the bile duct bifurcation and the distal retropancreatic duct is primarily lateral in arrangement, whereas the blood supply to the supraduodenal portion of the bile duct has a primarily axial or longitudinal pattern. The so-called 3- and 9-o’clock arteries and other small vessels arise from the right hepatic artery and the retroduodenal artery, which is a branch of the gastroduodenal artery, and form the skeleton of a pericholedochal plexus of vessels. An additional source of blood supply to the common bile duct can be the retroportal artery. This vessel arises from the celiac axis or the superior mesenteric artery and generally joins the retroduodenal artery; however, in approximately one third of individuals it ascends the back of the common bile duct to the right hepatic artery. The portion of the bile duct supplied by the longitudinal vessels receives most of its arterial blood supply from below, thus rendering the proximal portion of the duct subject to ischemia after injury or transection.
Answer
A
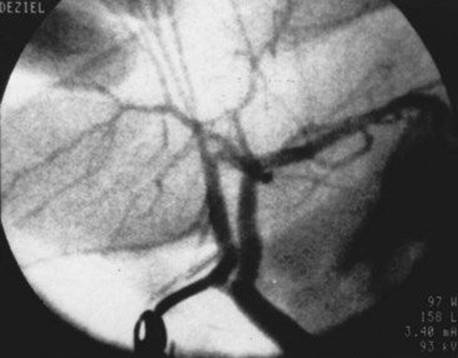
4 In this intraoperative cholangiogram, the arrow points to what duct?
A Common hepatic duct
B Accessory right hepatic duct
C Separately inserting right sectional duct
D “Crossover” right hepatic duct
E Cystic duct
Ref.: 2, 4, 5
Comments
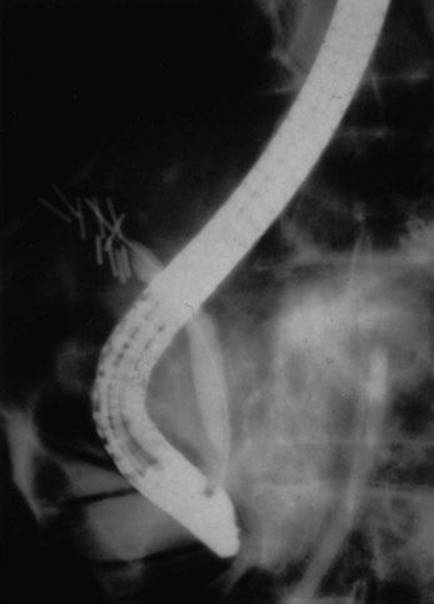
Variations in the anatomy of the extrahepatic bile ducts occur commonly. The surgeon must be cognizant of these variations and learn to recognize and identify them to prevent inadvertent injury to the bile ducts during cholecystectomy. Approximately two thirds of individuals have the “textbook” anatomy, with the anterior (segments V and VIII) and posterior (segments VI and VII) sectional ducts from the right joining to form the main right hepatic duct, which then joins the main left hepatic duct to form the common hepatic duct. In 15% to 25% of individuals, the anterior or posterior sectional duct from the right lobe inserts separately into the common hepatic duct. When the posterior duct inserts separately, it is usually at a greater distance caudally from the junction of the left duct and the other right duct than when the anterior duct inserts separately. This duct is therefore at risk for injury during cholecystectomy if the anatomy is not recognized.
One of the most common variations in cystic duct anatomy is direct insertion into one of these separately inserting right hepatic ducts, as the pictured cholangiogram demonstrates. The terms “crossover duct” and “accessory duct” are misnomers for this arrangement. True accessory ducts are rare and occur when there is embryologic duplication of the bud that forms the bile ducts and liver.
Answer
C
5 In this longitudinal laparoscopic ultrasound scan of the hepatoduodenal ligament, what structure is labeled B?
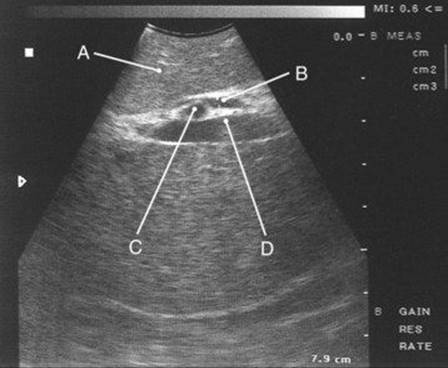
A Portal vein
B Common hepatic artery
C Right hepatic artery
D Common bile duct
E Right hepatic duct
Ref.: 6
Comments
See Question 6.
Answer
D
6 In this transverse laparoscopic ultrasound scan of the hepatoduodenal ligament, which structure is labeled B?
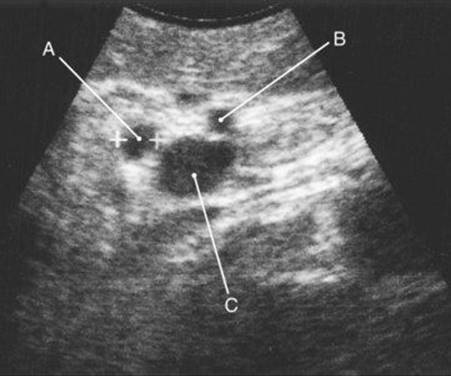
A Portal vein
B Common hepatic artery
C Right hepatic artery
D Common hepatic artery
E Right hepatic duct
Ref.: 6
Comments
A general principle of ultrasonography is that any structure visualized in one plane should also be examined in a second plane at a 90-degree angle to the first view to ascertain where and what the structure is. Intraoperative ultrasound imaging, whether laparoscopic or open, is an accurate method for identifying bile duct anatomy and assessing the bile duct for stones during cholecystectomy. The longitudinal and transverse scans of the hepatoduodenal ligament in Questions 5 and 6 depict typical anatomy. In the longitudinal plane, the common bile duct appears as a hypoechoic, tubular structure parallel and anterior to the portal vein. The normal upper-limit diameter of the duct at this location is 6 mm by ultrasound imaging criteria. In other words, a nondilated duct should not exceed one half the diameter of the neighboring portal vein. The right hepatic artery most commonly crosses behind the bile duct and is viewed in cross section on the longitudinal scan. In the transverse plane, the structures of the hepatoduodenal ligament have a “Mickey Mouse” configuration. The cross sections of the bile duct and common hepatic artery appear as smaller hypoechoic circles anterior to the larger portal vein. The structures labeled in the scan from Question 5 are as follows: A, liver; B, common bile duct; C, right hepatic artery; D, portal vein. The structures labeled in the scan from Question 6 are as follows: A, common bile duct; B, common hepatic artery, C, portal vein.
Answer
B
7 If a patient has complete bile duct obstruction, which of the following does not occur?
A Triglyceride absorption
B Vitamin K absorption
C Cholesterol synthesis
D Bilirubin conjugation
E All of the above
Ref.: 4
Comments
Bile has a number of critical functions related to the digestion and absorption of fats and the elimination of various endogenous and exogenous substances. Bile interacts with pancreatic lipase and colipase in the intraluminal hydrolysis of dietary triglycerides. It subsequently solubilizes the monoglycerides and fatty acids produced by triglyceride metabolism by forming mixed micelles. The micelles facilitate mucosal uptake of triglycerides by permitting transport across the water barrier adjacent to the enterocyte membrane. Although bile therefore plays an important role in triglyceride absorption, a substantial amount of triglycerides can be absorbed, even in the absence of bile, because of the long length of the intestine. The same is not true for the fat-soluble vitamins A, D, E, and K, which are minimally water soluble and are not absorbed in any substantial amount in the absence of micelles. Patients with long-standing cholestasis generally require supplementation of these fat-soluble vitamins to prevent the clinical effects of deficiency. Bile is the sole pathway for elimination of bilirubin and cholesterol from the body. Bilirubin is secreted into hepatic bile by an active transport mechanism following hepatic uptake and conjugation. Cholesterol is eliminated both by synthesis of bile acids from cholesterol and by solubilization of cholesterol in bile during secretion.
Answer
B
8 What change in bile flow would be expected in a patient with an external biliary fistula?
A Increased total canalicular flow
B Decreased bile acid–dependent canalicular flow
C Increased bile acid–dependent canalicular flow
D Decreased bile acid–independent canalicular flow
E Increased bile acid–independent canalicular flow
Ref.: 2, 4
Comments
Approximately 600 mL of hepatic bile are produced daily. Seventy-five percent of hepatic bile is formed by the bile canaliculi, and the remainder is secreted by the ducts. Canalicular bile can be divided into approximately equal bile acid–dependent and bile acid–independent fractions. The bile acid–dependent fraction results from active secretion of bile acids by the hepatocyte. This secretion depends on intestinal absorption and enterohepatic circulation of bile acids. Patients with external bile losses therefore have reduced bile acid–dependent canalicular flow and consequently reduced total canalicular flow. The bile acid–independent portion of canalicular flow is the result of secretion of inorganic electrolytes. Ductular secretion modifies canalicular bile flow by adding fluid and inorganic electrolytes.
Answer
B
9 Cholic acid is converted by bacteria to which of the following secondary bile acids?
A Deoxycholic acid
B Chenodeoxycholic acid
C Lithocholic acid
D Ursodeoxycholic acid
E None of the above
Ref.: 2-4, 7
Comments
The primary human bile acids cholic acid and chenodeoxycholic acid are synthesized from cholesterol in the liver. The secondary bile acids deoxycholic acid and lithocholic acid are formed in the intestine as the result of bacterial enzyme activity. 7-Ketolithocholic acid is also a secondary bile acid. It is converted to the tertiary bile acid ursodeoxycholic acid in the liver.
Answer
A
10 Conjugated bile acids are primarily absorbed in the intestine by which of the following mechanisms?
A Active transport in the colon
B Passive transport in the colon
C Active transport in the ileum
D Passive transport in the ileum
E Bacterial translocation
Ref.: 2-4, 7
Comments
Enterohepatic cycling of bile acids begins at the hepatocyte level. Bile acids are conjugated in the liver with glycine or taurine, secreted into the biliary system, concentrated and stored in the gallbladder, and then delivered to the duodenum after gallbladder contraction. Most bile acids are efficiently resorbed in the intestine. The site and mechanism of intestinal absorption differ according to the form of the bile acid and its corresponding lipid solubility. Conjugated bile acids are predominantly ionized in the intestinal pH range and are relatively lipid insoluble. Conjugated forms are therefore absorbed by an active transport mechanism in the terminal ileum. This mechanism accounts for approximately 70% to 80% of the enterohepatic circulation. Bacterial deconjugation of bile acids occurs in the colon and small intestine, as does conversion of primary bile acids to secondary forms. Deconjugation raises the pKaof bile acids and enables resorption by passive non-ionic diffusion, which occurs predominantly in the colon but to some extent in the small intestine as well. Both primary and secondary bile acids are resorbed and taken back to the liver. Unconjugated forms are then reconjugated and resecreted. Hepatic bile therefore contains both primary and secondary bile acids, with the primary bile acids normally constituting 60% to 90% of the total bile pool. Hepatic synthesis of new bile acids approximates fecal losses of 300 to 600 mg/day.
The bile acid pool cycles four to eight times per day, and hepatic secretion is dependent on enteral return. Disruption of this cycle therefore diminishes bile acid secretion. Clinical conditions that may be associated with bile acid malabsorption include ileal disease or resection, small bowel dysmotility or obstruction, and blind loop syndrome. Clinical consequences of this disordered physiology may include fat malabsorption, deficiencies of fat-soluble vitamins (A, D, E, and K), choleretic diarrhea caused by impaired colonic water absorption by bile acids, and formation of gallstones.
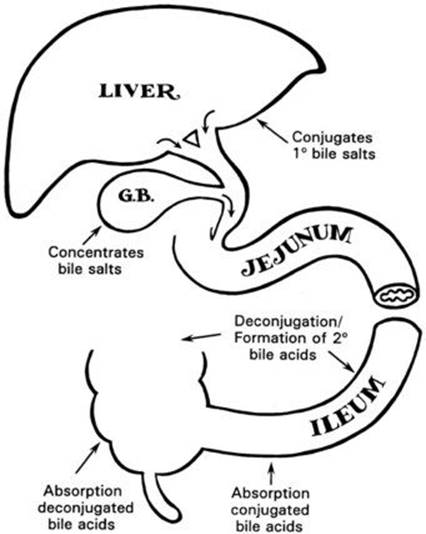
G.B., Gallbladder; 1°, primary; 2°, secondary.
Answer
C
11 Normal functions of the gallbladder epithelium include all but which of the following?
A Absorption of water
B Absorption of sodium and chloride
C Absorption of conjugated bile acids
D Secretion of hydrogen ion
E Secretion of glycoproteins
Ref.: 3, 7
Comments
The primary functions of the gallbladder are to concentrate and store bile between feedings. The gallbladder epithelium absorbs solutes and water across concentration gradients by both active and passive mechanisms. The main concentrating force is active absorption of sodium (coupled to chloride transport), which leads to passive absorption of water. Abnormalities in gallbladder absorption are part of the pathophysiologic process of gallstone formation. Absorption of organic solutes is normally minimal and depends on their lipid solubility. Unconjugated bile acids are more lipid soluble than their conjugated forms. Absorption of unconjugated bile acids that form in the presence of bacteria or inflammation damages the mucosa, thereby promoting absorption of other solutes and destabilizing cholesterol in solution. The gallbladder epithelium is also secretory. Secretion of hydrogen ion lowers the pH of gallbladder bile in relation to hepatic bile. Mucin glycoproteins secreted by the mucosa may have both a protective function and a critical role as a nucleating factor during gallstone formation.
Answer
C
12 Which of the following usually produces gallbladder contraction?
A Adrenergic stimulation
B Vasoactive intestinal peptide (VIP)
C Somatostatin
D Cholecystokinin (CCK)
E Secretin
Ref.: 3
Comments
Gallbladder function is subject to many neurohormonal influences. Generally, stimulation of parasympathetic vagal nerves causes gallbladder contraction, and stimulation of sympathetic nerves from the celiac ganglion causes gallbladder relaxation. Regulation of gallbladder function is actually a complex process that involves the interaction of various neural, hormonal, and peptidergic stimuli on various receptors located on the gallbladder muscle, blood vessels, and nerves. Cholinergic stimuli (including vagal) and CCK cause contraction. CCK receptors can be found on both gallbladder smooth muscle cells and intrinsic cholinergic nerves. Adrenergic stimulation (sympathetic) usually causes relaxation, but selective stimulation of certain adrenergic receptors can cause contraction. VIP and somatostatin inhibit gallbladder contraction, which can account for clinical biliary manifestations in patients with tumors that secrete those substances or in patients being administered somatostatin agonists. Many other peptides, hormones, and neurotransmitters may also affect gallbladder function, although their clinical significance is not completely known.
Answer
D
13 Which of the following is true regarding gallbladder emptying in between meals?
A It does not occur.
B It is stimulated by CCK.
C It is inhibited by CCK.
D It depends on peristalsis of the common bile duct.
E It is stimulated by motilin.
Ref.: 3, 7
Comments
Bile flow in the biliary tract varies according to the fasting or fed state of the individual. Cholecystokinin, which is released by the duodenum in response to the ingestion of food substances, facilitates delivery of bile to the intestine by stimulating contraction of the gallbladder and relaxation of the sphincter of Oddi. Normal contraction of the gallbladder in response to meals results in approximately 80% emptying in 2 hours. The common bile duct is for the most part a passive conduit in humans and does not play an active role in biliary motility. Filling of the gallbladder after it has emptied depends on neural and hormonal factors that relax the gallbladder and increase resistance of the sphincter of Oddi. During the interdigestive period, the gallbladder gradually fills, but this filling is interrupted by cyclic periods of emptying, during which time approximately one third of the gallbladder volume is dispensed. This cyclic pattern during fasting is correlated with the interdigestive myoelectric migratory complex of the intestine and is related to increased levels of plasma motilin. Motilin is a 21–amino acid peptide, and plasma motilin levels vary cyclically during the fasting period.
Answer
E
14 Which of the following levels of enzyme activity is most likely to be present in a nonobese individual with cholesterol gallstones?
A Increased 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase activity
B Decreased HMG-CoA reductase activity
C Increased 7α-hydroxylase activity
D Decreased 7α-hydroxylase activity
E Decreased enterokinase activity
Ref.: 2
Comments
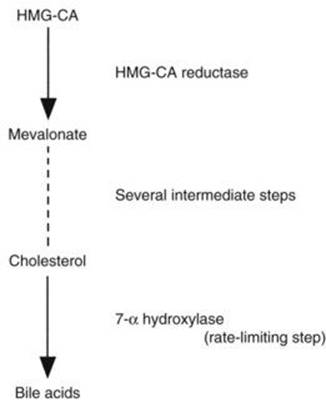
Cholesterol solubility in bile depends on the concentration of cholesterol relative to bile acids and phospholipids. Although an increase in hepatocyte cholesterol synthesis and secretion has been implicated in obese patients with gallstones, a relative deficiency of bile acid secretion is thought to be responsible for gallstone formation in many nonobese patients. HMG-CoA reductase catalyzes the conversion of HMG-CoA to mevalonate and is the early rate-limiting enzyme in cholesterol synthesis. The primary bile acids are formed from cholesterol, and the rate-limiting enzyme in this process is 7α-hydroxylase. Relative imbalances in the activities of these enzymes therefore affect cholesterol solubility in bile.
Answer
D
15 Which of the following is decreased after cholecystectomy?
A Size of the bile acid pool
B Rate of enterohepatic recycling
C Rate of bile acid secretion
D Cholesterol solubility in bile
E Rate of bilirubin conjugation
Ref.: 2
Comments
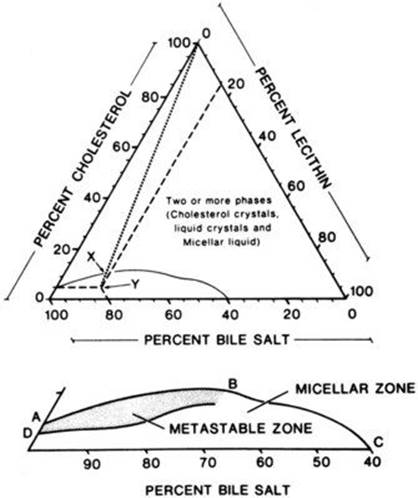
The total size of the bile acid pool is diminished after cholecystectomy as a result of loss of the gallbladder reservoir. However, cholecystectomy produces a more continuous flow of bile into the intestine, which increases the frequency of enterohepatic cycling and stimulates bile acid secretion. For these reasons, even though the size of the bile acid pool is diminished, cholecystectomy improves cholesterol solubility in bile. The solubility of cholesterol in bile depends on the relative molar concentration of cholesterol in relation to the concentration of bile acids and the phospholipid lecithin. This relationship, described by W. Admirand and D. M. Small in 1969, is graphically depicted by the following familiar diagram:
Answer
A
16 Which of the following is the primary form in which cholesterol is transported in bile?
A Dissolved as free cholesterol
B Dissolved as conjugated cholesterol
C Attached to a protein carrier
D Solubilized in mixed micelles
E Solubilized in phospholipid vesicles
Ref.: 3, 7
Comments
Cholesterol is insoluble in water, and bile is a solution composed of 90% water. The solubility of cholesterol in bile depends on the presence of bile acids and the phospholipid lecithin. These molecules aggregate into physicochemical structures that shelter cholesterol within a nonpolar, hydrophobic center and thus permit dissolution. For many years, the mixed micelle was recognized as the structure principally responsible for cholesterol solubility. Subsequently, it has been found that most cholesterol is usually solubilized in larger bilayered lipid structures known as vesicles. The balance between micelles and vesicles is a dynamic process. Recognition of these vesicles is particularly important because crystallization of cholesterol to form stones occurs from this phase.
Answer
E
17 Which of the following is not part of the process of cholesterol gallstone formation?
A Supersaturation of bile with cholesterol
B Bilirubin deconjugation
C Crystal nucleation
D Aggregation of cholesterol monomers
E Stone growth
Ref.: 2, 3, 7
Comments
Cholesterol gallstone formation is a complex physicochemical process. The requisite steps in the genesis of cholesterol stones can be conceptually simplified as cholesterol saturation, nucleation, and stone growth. The cholesterol content of bile must exceed the capacity for bile to solubilize cholesterol in vesicles and micelles. Cholesterol supersaturation alone, however, is not sufficient to cause stones because this process can occur in normal individuals. Nucleation must also take place; that is, cholesterol monohydrate crystals must form and aggregate. Finally, the crystals must enlarge by fusion or continued solid deposition to produce a stone large enough to be clinically relevant. Bacterial infection is thought to be an important pathogenic factor in the development of some pigment stones but not generally cholesterol stones. Bacterial infection is associated with deconjugation of bilirubin and subsequent formation of insoluble calcium bilirubinate complexes. Bacterial infection can also result in the production of glycocalyx, an adhesive glycoprotein that plays a role in pigment stone formation.
Answer
B
18 Nucleation during cholesterol gallstone formation involves all but which of the following?
A Mixed micelles
B Biliary vesicles
C Biliary calcium
D Gallbladder stasis
E Mucus secretion
Ref.: 3, 7
Comments
Nucleation, or the formation and aggregation of solid cholesterol monohydrate crystals, is a necessary step in gallstone formation. There are factors that promote nucleation and some antinucleating factors that may protect against stone formation. Mucin glycoproteins secreted by the gallbladder epithelium are thought to be key nucleating factors. Increased mucus secretion occurs whenever there is gallbladder stasis, and this precedes the development of cholesterol crystals. Prostaglandins stimulate mucus production in animal models, and prostaglandin inhibitors can prevent stones. Nucleation is associated with the vesicular fraction of bile rather than with the mixed micelles. Biliary calcium also plays a role in the formation of both cholesterol and pigment stones. Calcium levels in gallbladder bile are increased during cholesterol stone formation. Calcium affects the absorptive function of the gallbladder epithelium and also promotes nucleation from vesicles. An understanding that the events of vesicle fusion, nucleation, and stone growth occur in the gallbladder is the basic foundation for cholecystectomy as the definitive treatment of cholesterol gallstone disease.
Answer
A
19 Cholesterol gallstones are associated with all except which of the following?
A Obesity
B Rapid weight loss
C Total parenteral nutrition (TPN)
D Exogenous estrogen
E High-calorie diet
Ref.: 2, 3
Comments
Changes in bile composition that either increase the relative concentration of cholesterol or decrease the relative concentration of bile acids favor cholesterol gallstone formation. Situations that lead to increased hepatocyte cholesterol secretion include obesity, rapid weight loss, diets high in calories and polyunsaturated fats, and estrogen therapy. Drugs that inhibit HMG-CoA reductase are used to treat hypercholesterolemia and may prevent gallstone formation. Theoretically, a relative decrease in the size of the bile acid pool would predispose a person to cholesterol gallstone formation in situations in which there were excessive bile acid losses (e.g., ileal disease or resection) or decreased bile acid synthesis (e.g., reduced 7α-hydroxylase activity). Stones associated with ileal disease or resection are of the pigment type, however. TPN is also associated with pigment gallstones in a high proportion of patients, depending on the duration of therapy.
Answer
C
20 Which of the following is the main chemical component of pigment gallstones?
A Cholesterol
B Calcium bilirubinate
C Calcium carbonate
D Calcium phosphate
E Calcium oxalate
Ref.: 2, 7
Comments
Pigment gallstones are composed primarily of calcium precipitated with bilirubin, carbonate, phosphate, or palmitate anions. Two relatively distinct types of pigment gallstones are recognized: black pigment gallstones and brown pigment gallstones. There are differences between black and brown pigment gallstones in terms of gross appearance, chemical composition, pathogenesis, and clinical implications. Black pigment gallstones are small and spiculated. They contain calcium bilirubinate primarily in polymerized form, as well as calcium carbonate or phosphate. Brown pigment gallstones are soft and yellow-brown, are also composed primarily of calcium bilirubinate, but contain more calcium palmitate (fatty acid derived from lecithin) and cholesterol than do black stones. The oxalate salts of calcium play no role in gallstone disease.
Answer
B
21 Which of the following features is more characteristic of black pigment gallstones than brown pigment gallstones?
A Association with hepatic cirrhosis
B Association with bacterial infection
C Location in the common bile duct
D Treatment requiring bile duct drainage
E Higher risk for cholangitis
Ref.: 2, 3, 7
Comments
There are some important clinical differences between patients with black pigment gallstones and those with brown pigment gallstones. It is postulated that these stones form by different pathogenic mechanisms. Stasis and infection are critical factors in the formation of brown pigment gallstones. Bile culture results are positive in most patients with brown pigment gallstones, and scanning electron microscopy demonstrates bacterial colonies or casts within the stones. Brown pigment gallstones are found more frequently in the common bile duct than in the gallbladder. They occur in older patients with stasis and in postcholecystectomy patients.
Black pigment gallstones are thought to have a metabolic cause. They often occur in patients with cirrhosis or hemolysis. The precise role of stasis and infection in black stone formation remains unclear, however. Approximately 20% of patients with black pigment gallstones have positive bile culture results, and some investigators have demonstrated bacteria in black stones. A subset of patients with gallstones have combined features of both black and brown pigment gallstones. The important therapeutic implication in differentiating black from brown pigment gallstones is that patients with brown pigment gallstones may require a definitive biliary drainage procedure to prevent recurrence, whereas patients with black pigment gallstones may be treated successfully by cholecystectomy alone.
Answer
A
22 Which of the following sonographic findings is not a feature of gallstone disease?
A Hyperechoic intraluminal structure
B Mobility of the intraluminal structure
C Shadowing posterior to the structure
D Acoustic enhancement posterior to the structure
E Sonographic Murphy sign in acute cholecystitis
Ref.: 6
Comments
External ultrasound imaging has a sensitivity of about 95% for the diagnosis of gallstones. The three sonographic criteria for gallstones are (1) the presence of a hyperechoic intraluminal focus, (2) shadowing posterior to that focus, and (3) movement of the focus with changes in position of the patient. Problems in interpretation arise when all of these criteria are not fulfilled. For example, small stones may not shadow well, and impacted stones do not move. Ultrasound imaging may also fail to diagnose stones if the gallbladder cannot be visualized well because it is contracted or close to excessive bowel gas. For an optimal elective ultrasound scan, the gallbladder should be examined after the patient has fasted for about 6 hours. Posterior acoustic enhancement is a sonographic feature of hypodense structures such as cysts. The signals behind the structure are “whiter” because the sound wave energy is less attenuated as it passes through. The gallbladder itself is a cystic structure and demonstrates this phenomenon, whereas gallstones do the opposite. A sonographic Murphy sign refers to tenderness when the ultrasound transducer is placed over the gallbladder. This is a typical finding in a patient with gallstones and acute cholecystitis.
Answer
D
23 Ultrasound imaging reveals gallstones in an asymptomatic 50-year-old woman. Which of the following is the recommended treatment?
A Observation
B Laparoscopic cholecystectomy
C Open cholecystectomy
D Ursodeoxycholic acid
E Extracorporeal shock wave lithotripsy (ESWL)
Ref.: 2, 3, 7
Comments
The appropriate management of asymptomatic cholelithiasis is sometimes controversial. First, the physician must determine whether the patient is in fact asymptomatic, because gastrointestinal complaints other than pain may be attributable to biliary tract disease. It was formerly thought that symptoms would eventually develop in most patients with silent gallstones and that the risk for subsequent complications was high. Subsequent studies suggested that symptoms develop in about 1% to 2% of patients each year and that serious complications are relatively infrequent. The morbidity, mortality, and cost of intervention in these patients may exceed those of expectant therapy. The availability of laparoscopic cholecystectomy has not changed the basic indications for surgery, although it has probably altered the symptomatic threshold for surgical referral. Nonoperative pharmacologic dissolution and ESWL are neither definitive nor cost-effective.
Currently, therefore, the incidental finding of asymptomatic cholelithiasis is not an indication for therapy in most situations. Circumstances that may be exceptions and that merit consideration on an individual basis include (1) a transplant patient with anticipated immunosuppression because of the risk for sepsis, (2) anticipated long-term parenteral nutrition because of associated stasis and sludge formation, (3) anticipated pregnancy because of the possibility of becoming symptomatic as gallbladder emptying is impaired and because of the potential risk imposed on both the mother and fetus if complicated cholelithiasis occurs, (4) concurrent abdominal surgery for an unrelated problem because of the relative ease and safety of incidental cholecystectomy in most situations and in consideration of the potential for postoperative cholecystitis otherwise, and (5) bariatric operations because of the high incidence of gallstones associated with obesity and during rapid weight loss. In patients requiring massive intestinal resection, concomitant cholecystectomy has been recommended even when the gallbladder is normal because disease will probably develop during parenteral nutrition.
Answer
A
24 In patients with which of the following conditions is early elective cholecystectomy for symptomatic gallstones not indicated?
A Elderly status
B Diabetes mellitus
C Child class C cirrhosis
D TPN-induced gallstones
E Chronic renal failure
Ref.: 3
Comments
Patients with certain medical conditions are often considered to be at higher risk for morbidity and mortality from gallstone disease. Complications of cholelithiasis, such as sepsis, perforation, and choledocholithiasis, more frequently develop in elderly patients. They also have a higher mortality rate during emergency operations. Elective cholecystectomy can usually be performed safely in the elderly and is recommended for symptomatic patients. Although the supportive evidence has not always been conclusive, diabetic patients may also be at increased risk, particularly if emergency intervention is required, and should therefore be considered for early elective cholecystectomy. Gallstones develop in a high proportion of patients maintained on long-term TPN, and reports suggest that complications, emergency operations, and mortality are more frequent in this population as well. Early cholecystectomy is therefore indicated. Cholecystectomy is also indicated for patients with chronic renal failure, particularly if they are candidates for renal transplantation. Patients with hepatic cirrhosis, however, have high morbidity and mortality rates related to cholecystectomy, especially those with hepatocellular dysfunction and portal hypertension. Cholecystectomy should be approached with great caution in these circumstances and is usually reserved for patients with complications of cholelithiasis or for patients with substantial symptoms and less advanced hepatic disease (Child class A).
Answer
C
25 A patient with abdominal pain has a CCK-stimulated hepatobiliary iminodiacetic acid (HIDA) scan that demonstrates 25% gallbladder emptying. Ultrasound imaging of the gallbladder is normal. What is true regarding cholecystectomy in this situation?
A Cholecystectomy is not indicated because persistent or recurrent symptoms are likely.
B Cholecystectomy is indicated only if duodenal drainage yields cholesterol crystals or bilirubinate granules.
C Cholecystectomy can alleviate symptoms in most patients if the pain is episodic and located in the right upper part of the abdomen.
D Cholecystectomy improves symptoms in most patients regardless of the location or characteristics of the pain.
E When compared with operations on patients with gallstones, there is a greater chance that laparoscopic cholecystectomy will need to be converted to an open procedure.
Ref.: 3, 8
Comments
Surgeons are often confronted with the challenge of evaluating patients for abdominal pain that may or may not be of biliary origin. If the symptoms are typical of biliary “colic” and ultrasound imaging demonstrates gallstones, the situation is straightforward. However, when the symptoms are less typical (even the presence of gallstones) or when ultrasound imaging does not identify any abnormality, further evaluation is necessary to determine whether cholecystectomy is warranted. Other diagnoses must be excluded, and additional investigations may be appropriate, depending on the specific circumstances (e.g., esophagogastroduodenoscopy, computed tomography [CT], endoscopic retrograde cholangiopancreatography [ERCP], gastrointestinal contrast-enhanced studies, and colonoscopy).
Cholecystokinin-stimulated cholescintigraphy can be useful for identifying patients who may have symptoms as a result of motility disorders of the gallbladder. However, the test does not always reliably predict the long-term outcome of cholecystectomy. If the symptoms are more typical of biliary origin and findings on CCK scintigraphy are abnormal (<30% ejection), data suggest that most patients (>70%) can benefit from cholecystectomy. Histologic abnormalities of the gallbladder are found in a reasonable number of these patients. If the symptoms are less typical, the results of cholecystectomy cannot be expected to be as favorable, even though emptying is abnormal. Additional testing, such as repeated ultrasonography or duodenal drainage with CCK cholecystography, might sometimes be useful for evaluating these patients.
Answer
C
26 Laparoscopic cholecystectomy is most strongly contraindicated in which of the following situations?
A Pregnancy
B Previous upper abdominal surgery
C Known common bile duct stones
D Chronic obstructive pulmonary disease
E Gallbladder cancer
Ref.: 3, 9
Comments
When laparoscopic cholecystectomy was first introduced worldwide during the late 1980s, there were a number of circumstances in which it was more or less strongly contraindicated. Today, most contraindications are relative, and in fact the laparoscopic approach is preferred when possible in certain situations that were initially considered contraindications (e.g., acute cholecystitis, choledocholithiasis, and obesity). Basically, the surgeon must be adequately trained and the patient reasonably fit for an operation and give informed consent that includes the possibility of laparotomy. It must be recognized that there are patients for whom the potential physiologic consequences of CO2pneumoperitoneum are more important, but the presence of underlying disease itself does not prohibit a laparoscopic approach. In fact, laparoscopic cholecystectomy may be more beneficial to the postoperative course of a compromised patient. Pregnancy is not a contraindication with appropriate precautions, although the physiologic effects on the fetus are not completely known. Perhaps the strongest contraindication currently involves patients with suspected or known gallbladder cancer because of the risk for dissemination.
Answer
E
27 Most major bile duct injuries during laparoscopic cholecystectomy occur in patients under which of the following circumstances?
A Acute cholecystitis
B Gallstone pancreatitis
C Choledocholithiasis
D Elective cholecystectomy
E Conversion of a laparoscopic procedure to an open procedure
Ref.: 10
Comments
There are several risk factors for bile duct injury during laparoscopic cholecystectomy. Pathologic risk factors include severe acute or chronic inflammation. Several studies have found a statistical correlation between the rate of duct injury and the presence of acute cholecystitis. Bleeding has long been implicated as a factor predisposing to duct injury during open or laparoscopic cholecystectomy. Injuries are sometimes attributed to the “anomalous” anatomy of the bile ducts. More often than not, however, such “anomalies” are simply common anatomic variations that the surgeon must recognize to prevent injury (see Question 4). The surgeon’s experience, or the “learning curve,” is clearly a risk factor, because higher rates of duct injury have been well documented in less experienced surgeons. It is interesting to note that there is no convincing evidence that duct injury is more frequent during cases involving laparoscopic management of common bile duct stones, possibly because these procedures are performed by more experienced surgeons. Unfortunately, most major bile duct injuries during laparoscopic cholecystectomy have occurred in elective and otherwise uncomplicated cases. Despite the presence or absence of risk factors, the primary problem resulting in duct injury is misidentification of the anatomy. The most frequent mechanism of injury is mistaking a major bile duct for the cystic duct and clipping and cutting it. This pitfall is best avoided by correct operative strategy, which means appropriate retraction and adequate dissection to obtain the “critical view of safety.” The critical view is achieved by dissecting the base of the gallbladder off the liver for an adequate distance to visualize the cystic plate and to verify that the only structures entering the gallbladder are the true cystic duct and the cystic artery. Intraoperative bile duct imaging with cholangiography or laparoscopic ultrasonography can also aid in discerning the anatomy. If the cystic duct cannot be conclusively identified, the surgeon must resort to alternative approaches such as laparoscopic subtotal cholecystectomy, conversion to an open operation, or termination of the procedure.
Answer
D
28 A surgeon encounters difficulty during an elective laparoscopic cholecystectomy in a healthy 25-year-old woman and converts to an open procedure. The 4-mm common hepatic duct has been transected 1 cm below the bifurcation. Which of the following procedures is the most appropriate?
A Duct-to-duct repair over a T tube
B Duct-to-duct repair without a stent
C Roux-en-Y hepaticojejunostomy
D Hepaticoduodenostomy
E Ligation of the duct and placement of a drain
Ref.: 11
Comments
When a transection or resection injury of the extrahepatic biliary tree is discovered at the time of cholecystectomy, the surgeon must make some careful decisions. Repair at the time is preferable, provided that the surgeon is adequately experienced in performing such a repair so that a successful outcome is likely. Unfortunately, the weight of evidence indicates that most primary repairs by the initial operating surgeon have failed, thus necessitating repeated operations and other interventions. The initial repair of a major duct injury has the best chance for long-term success. A less experienced surgeon should not attempt anastomosis of a small bile duct but seek the help of an experienced colleague if available. Otherwise, drains should be placed and transfer to an experienced hepatobiliary surgeon arranged. If repair at the time is appropriate, the standard reconstruction for this type of injury is a Roux-en-Y hepaticojejunostomy. Duct-to-duct repairs usually fail in this situation. Hepaticoduodenostomy is not recommended for an injury at this level.
Answer
C
29 How would the bile duct injury described in Question 28 be classified?
A Bismuth type 1
B Bismuth type 2
C Bismuth type 3
D Bismuth type 4
E Bismuth type 5
Ref.: 4
Comments
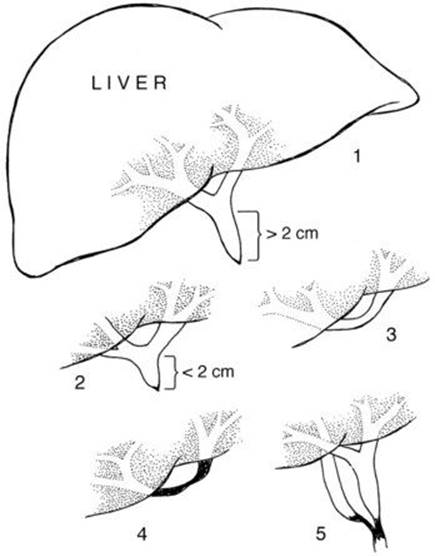
The Bismuth classification of bile duct injuries and strictures describes the level of injury in relation to the bifurcation of the main right and left hepatic ducts. Higher injuries are more difficult. They require a greater degree of technical skill and expertise to reconstruct, and reconstructions may have a lower long-term success rate. Many of the injuries resulting from laparoscopic cholecystectomy have been higher than those seen with open cholecystectomy. Moreover, many injuries, initially lower, end up being higher when repaired because of the need to débride unhealthy ductal tissue as a result of ischemia or inflammation and infection caused by bile leakage. With a type 1 injury, 2 cm or more of the common hepatic duct is preserved below the bifurcation. With a type 2 injury, less than 2 cm remains. A type 3 injury reaches the bifurcation with preservation of continuity between the right and left ducts. A type 4 injury involves destruction of the hepatic duct confluence with separation of the right and left hepatic ducts. A type 5 injury involves a separate inserting right sectoral duct with or without injury to the common duct.
Answer
B
30 On the second postoperative day following elective laparoscopic cholecystectomy, a 40-year-old woman complains of nausea and abdominal pain. Examination shows a temperature of 100° F (37.8° C), a pulse of 100 beats/min, mild abdominal distention, and moderate right upper quadrant tenderness. Which of the following would next be appropriate?
A Administration of intravenous antibiotics
B Magnetic resonance cholangiopancreatography (MRCP)
C HIDA scan
D ERCP
E Percutaneous transhepatic cholangiography (PTC)
Ref.: 11, 12
Comments
Serious delays in the postoperative diagnosis of bile duct injuries can compound a patient’s problems. A patient should be investigated promptly when the clinical course suggests anything other than the anticipated straightforward recovery that most patients experience. The primary concern is development of a bile leak, which occurs in 1% to 2% of patients. Other problems, such as retained bile duct stones or intestinal injury, can occur as well, although they are less frequent.
The various imaging studies can provide complementary information. An HIDA scan shows an ongoing bile leak and is often the most reasonable initial investigation after the patient is examined. Ultrasound or CT can demonstrate fluid collections or intrahepatic bile duct dilation. If a fluid collection is seen, percutaneous aspiration can determine whether the fluid is bile. If a bile leak is confirmed, cholangiography is necessary to establish the site of leakage and help determine further therapy. Endoscopic cholangiography is generally the first choice and may be all that is necessary for bile leaks that originate from lateral injuries, the cystic duct stump, or the gallbladder fossa. Percutaneous transhepatic cholangiography is necessary for complete anatomic definition in patients with transection or resection injuries or injuries to sectoral hepatic ducts that may not be in continuity with the rest of the extrahepatic bile ducts. MRCP is not an initial diagnostic examination but can be useful for delineation of bile duct anatomy in complex situations.
Answer
C
31 A stable patient underwent endoscopic cholangiography following laparoscopic cholecystectomy 2 days previously. What should be done next?
A Endoscopic balloon dilation and stent placement
B PTC
C Reoperation for bile drainage
D Reoperation for bile duct reconstruction
E Percutaneous catheter drainage
Ref.: 11, 13, 14
Comments
The endoscopic cholangiogram demonstrates complete occlusion of the supraduodenal common bile duct without extravasation of dye. A classic mechanism of major bile duct injury during laparoscopic cholecystectomy involves clipping the distal common bile duct and resecting a portion of the extrahepatic ductal system. The proximal level of injury is variable but typically high. Bile leakage or obstruction occurs, depending on the status of the proximal ducts. The first priority when managing these injuries is to control sepsis and ensure adequate drainage of any bile leak. Generally, this can be accomplished by nonoperative percutaneous or endoscopic methods. Urgent reoperation for bile drainage is not typically necessary. Complete cholangiographic definition of the injury is recommended before definitive repair. For resection or transection injuries, as depicted above, PTC is used to assess the status of the proximal ducts. Endoscopic cholangiography alone may be adequate for lateral injuries when the continuity of the ducts is preserved. Occasionally, a “fistulogram” done through a percutaneous drainage catheter may visualize the proximal ducts. After complete cholangiography, long-term success is best achieved by an elective, expert reconstruction.
Answer
B
32 Which of the following is true regarding the use of intraoperative cholangiography (IOC) and bile duct injury during laparoscopic cholecystectomy?
A Selective use of IOC effectively prevents bile duct injury.
B Routine use of IOC effectively prevents bile duct injury.
C Selective use of IOC is associated with a higher rate of bile duct injury.
D The severity of bile duct injury is independent of the use of IOC.
E Use of IOC increases the intraoperative diagnosis of injury.
Ref.: 15
Comments
As long as there are imaging studies to assess the bile ducts intraoperatively, the debate between proponents of routine versus selective use of such studies will continue. Proponents of IOC argue that its routine or liberal use can be advantageous in terms of bile duct injury and that there is an association between routine IOC and lower rates of duct injury. Cholangiograms can be incomplete or misinterpreted, however, and injuries can occur after IOC has been done. Properly performed IOC does not cause duct injury. There is a compelling argument that IOC may limit the severity of duct injury. For example, IOC may allow a surgeon to recognize that the cholangiogram catheter has been placed in the common duct and not the cystic duct before transection of the common duct. Some evidence suggests that the number of high duct injuries and anastomotic repairs required to remedy duct injuries has been lower when IOC was performed. The use of IOC increases the intraoperative recognition of any injury that has occurred. About 70% to 90% of injuries have been identified intraoperatively when IOC has been performed as compared with only 15% to 25% when IOC has not been done. Failure to interpret the results of IOC correctly can account for missed injuries. The two primary reasons for misinterpreting the results of IOC are failure to completely visualize the proximal ducts (including both the right anterior and posterior ducts) and extravasation of dye of uncertain origin.
Answer
E
33 Which of the following is an early event in the pathophysiology of acute calculous cholecystitis?
A Increased biliary lysolecithin
B Gallbladder ischemia
C Bacterial infection
D Prostaglandin depletion
E CCK receptor depletion
Ref.: 3, 7
Comments
Acute cholecystitis is thought to be initiated by gallbladder obstruction and activation of various inflammatory mediators, which lead to mucosal damage, gallbladder distention, and eventually ischemia. Bacteria can be identified in the bile of about 50% (30% to 70%) of patients with acute cholecystitis, but bacterial infection is a secondary phenomenon. The primary pathophysiology depends on the biochemical events that take place. Some of the mediators that may be involved in the inflammatory process of acute cholecystitis are bile acids, lithogenic bile, pancreatic juice, prostaglandins, phospholipids, and lysolecithin. Lysolecithin is formed from lecithin by the enzyme phospholipase, and levels are elevated in patients with acute cholecystitis. The role of prostaglandins as mediators in this process has also received considerable attention.
Answer
A
34 Which of the following is most accurate in the diagnosis of acute cholecystitis?
A Plain abdominal radiographs
B Ultrasound imaging
C Oral cholecystography
D Technetium-99m pertechnetate and HIDA scans
E Leukocytosis with elevated transaminases
Ref.: 2, 3
Comments
Radionuclide scanning with 99mTc-iminodiacetic acid agents normally allows visualization of the liver, gallbladder, and extrahepatic biliary tree. In the presence of acute cholecystitis, the gallbladder cannot be seen because of obstruction of the cystic duct. This finding is present in approximately 98% of patients with acute cholecystitis. Cholescintigraphy is not necessary in most patients with acute cholecystitis because the diagnosis is founded on clinical examination and demonstration of gallstones by ultrasound imaging. However, it can be quite useful in less typical situations and to exclude acute cholecystitis (by normal gallbladder uptake) in patients with other diagnoses. Ultrasound imaging of acute cholecystitis may demonstrate gallstones, pericholecystic fluid, thickening of the gallbladder, intramural edema, or a positive sonographic Murphy sign, but the morphologic findings are not specific. Although oral cholecystography fails to allow visualization of the gallbladder in patients with acute cholecystitis, this technique is not as diagnostically reliable as a radioisotope study because of the high frequency of gallbladders that cannot be visualized as a result of impaired dye absorption, hepatic uptake, or the presence of chronic cholecystitis. Plain abdominal radiographs reveal up to 15% of gallstones and demonstrate emphysematous cholecystitis but otherwise play no specific role in the diagnosis of acute cholecystitis. Elevations of the white cell count and transaminases are nonspecific.
Answer
D
35 A 99mTc-iminodiacetic acid scan in a fasting patient demonstrates the following: normal liver activity, no gallbladder visualization at 60 minutes, intestinal activity present at 60 minutes, and gallbladder visualization at 120 minutes. These findings are most consistent with which of the following situations?
A Normal study results
B Acute calculous cholecystitis
C Acute acalculous cholecystitis
D Chronic cholecystitis
E Partial bile duct obstruction
Ref.: 2, 3
Comments
Since the mid-1970s, technetium-labeled derivatives of iminodiacetic acid (i.e., HIDA, PIPIDA, and DISIDA) have been important in the evaluation of biliary tract disease. After intravenous injection, these radioisotopes are taken up by the liver and excreted into the biliary tract. The characteristics of a normal study include visualization of the gallbladder within 60 minutes in fasting patients and the appearance of radioisotope in the duodenum by about the same time. In nonfasting patients, visualization of the gallbladder may be delayed. The hepatic phase of the study may demonstrate mass lesions or diminished uptake in patients with hepatic dysfunction. Such results are similar to those of a liver scan. With both calculous and acalculous acute cholecystitis, the gallbladder is not visualized because of cystic duct obstruction. No visualization or delayed visualization is common with chronic cholecystitis. The distinction between acute and chronic cholecystitis therefore depends on the clinical findings, not simply on abnormal scan results. Bile duct obstruction may cause delayed or absent clearance of isotope from the liver or delayed hepatic uptake. Radioisotope scans can be useful in the clinical assessment of disorders other than cholecystitis, including biliary motility, biliary enteric anastomosis, bile fistulas or leaks, and enterogastric reflux.
Answer
D
36 What is the preferred treatment of acute calculous cholecystitis?
A Early laparoscopic cholecystectomy
B Delayed laparoscopic cholecystectomy
C Early open cholecystectomy
D Delayed open cholecystectomy
E Intravenous antibiotics
Ref.: 2, 3
Comments
The former debate over early versus late cholecystectomy for acute cholecystitis has for the most part been put to rest. Prospective studies have demonstrated that early cholecystectomy within the first few days is not associated with higher morbidity or mortality and that delayed surgery requires longer hospitalization, is more expensive, and risks recurrent biliary problems before definitive therapy. Most patients are treated effectively by stabilization and prompt surgery. From a technical standpoint, cholecystectomy is often easier during the first day or two of the patient’s illness, when the inflammation tends to be more edematous rather than necrotic and hyperemic, as it becomes when the process progresses. Laparoscopic cholecystectomy is the preferred treatment in most circumstances, although conversion to an open procedure is required more often than when the procedure is performed electively for nonacute symptoms.
Answer
A
37 With regard to acalculous cholecystitis, which of the following statements is true?
A It most commonly affects elderly patients in an outpatient setting.
B The primary pathophysiologic feature involves gallbladder stasis.
C HIDA scan results are usually normal.
D Ultrasound imaging of the gallbladder is usually normal.
E Treatment requires cholecystectomy.
Ref.: 2, 3
Comments
Approximately 5% to 10% of acute cholecystitis cases occur in patients without gallstones. The primary predisposing factor is gallbladder stasis with subsequent distention and ischemia. Acalculous cholecystitis typically develops in hospitalized patients, often after trauma, unrelated surgery, or other critical illnesses. Factors present in these patients that may contribute to biliary stasis include hypovolemia, intestinal ileus, absence of oral nutrition, multiple blood transfusions, narcotic use, and positive pressure ventilation. Because of the clinical situation in which acute acalculous cholecystitis occurs, the diagnosis may not be readily apparent. The patient may have fever or unexplained sepsis, and abdominal signs may not be initially appreciated. The results of imaging studies are generally abnormal. Because of stasis and functional obstruction of the cystic duct, HIDA scanning fails to allow visualization of the gallbladder, and ultrasonography may demonstrate sludge, thickening of the gallbladder wall, or pericholecystic fluid. None of these findings is specific for the presence of acute acalculous cholecystitis, however, and the diagnosis must rely on clinical suspicion.
Standard surgical treatment consists of cholecystectomy (or cholecystostomy for patients who are too infirm to withstand general anesthesia). Percutaneous cholecystostomy can be a valuable technique for establishing gallbladder decompression in these critically ill patients. Later cholecystectomy may not be required if stones are not present and subsequent cholangiography demonstrates a patent cystic duct. Cholecystectomy is the only effective treatment if the gallbladder is necrotic or gangrenous.
Answer
B
38 The pertinent area of a plain x-ray film of the abdomen of a 78-year-old diabetic man with right upper quadrant pain is shown below. Which of the following is the appropriate next step?
A Ultrasound imaging of the gallbladder
B CT
C HIDA scan
D Cholecystectomy
E ERCP

Ref.: 2, 3
Comments
Emphysematous cholecystitis occurs most typically in elderly diabetic men. Curvilinear radiolucencies in the right upper quadrant have the configuration of the gallbladder, are in the location of the gallbladder, and are diagnostic of gas in the gallbladder wall. In their totality, they are pathognomonic of emphysematous cholecystitis. Gas may also be seen in the gallbladder lumen. This condition is associated with a high incidence of gallbladder necrosis, perforation, and sepsis. Unnecessary diagnostic examinations would only delay prompt surgical therapy and possibly affect the outcome adversely. Urgent surgery is needed. An ultrasound study of an emphysematous gallbladder would show highly reflective shadows as a result of the gas. Differentiation from bowel gas may be difficult, although the diagnosis is usually evident. About one third of patients do not have stones. CT would show the abnormal gas in the gallbladder wall, lumen, or both. HIDA scans would fail to allow visualization of the gallbladder. ERCP is unnecessary.
Answer
D
39 A 24-year-old woman who is 10 weeks pregnant is hospitalized with gallstone pancreatitis and recovers after 2 days of nonoperative management. Which of the following recommendations is the most appropriate?
A Laparoscopic cholecystectomy before discharge
B Open cholecystectomy before discharge
C Laparoscopic cholecystectomy in 4 weeks
D Open cholecystectomy in 4 weeks
E Nonoperative management until term and postpartum laparoscopic cholecystectomy
Ref.: 16
Comments
Symptomatic gallstone disease is second to appendicitis as the most common nonobstetric surgical problem that affects pregnant women. The overwhelming majority of women who become symptomatic during the first trimester of pregnancy will have continuing or recurrent symptoms before delivery. Without definitive treatment, rehospitalizations are frequent and there is ongoing risk to both the mother and fetus. This has been particularly so when biliary pancreatitis has been the symptomatic manifestation. Cholecystectomy is therefore indicated and is preferably performed during the second trimester of pregnancy if the clinical situation will allow. Laparoscopic cholecystectomyhas been performed successfully during all stages of pregnancy. In late term, however, the size of the gravid uterus interferes with trocar placement. For this reason, many surgeons prefer an open approach if surgery is necessary during the third trimester.
Answer
C
40 During a difficult laparoscopic cholecystectomy for acute cholecystitis, you recognize that the patient has hepatic cirrhosis and portal hypertension. Which of the following is the best option?
A Conversion to open cholecystectomy
B Completion of the laparoscopic cholecystectomy
C Laparoscopic subtotal cholecystectomy
D Terminating the procedure and arranging for transjugular intrahepatic portosystemic shunt (TIPS) surgery
E Placement of drains and termination of the procedure
Ref.: 17
Comments
See Question 41.
Answer
C
41 A patient has undergone subtotal cholecystectomy with a portion of the gallbladder infundibulum left in situ. On the second postoperative day, bile is coming from a subhepatic drain placed at the time of surgery. Which of the following is the most appropriate step?
A Endoscopic retrograde cholangiography
B PTC
C Removal of the drain
D Leaving the drain in place and monitoring
E Returning to the operating room for completion of the cholecystectomy
Ref.: 17
Comments
Safe management of a patient with a difficult laparoscopic cholecystectomy requires technical skill, considerable judgment, and familiarity with a spectrum of operative options. Such options include open cholecystectomy, “fundus first” cholecystectomy, laparoscopic or open cholecystostomy, and laparoscopic or open subtotal cholecystectomy. Alternatives to total cholecystectomy can help avoid major bile duct or vascular injury under difficult circumstances. Cholecystostomy tube placement can be lifesaving; potential disadvantages include tube complications, the possible need for a reoperation later, and possible inability to place a tube if the gallbladder is necrotic or gangrenous. Subtotal cholecystectomy can help avoid injury and bleeding and reduce the need for cholecystostomy and reoperation. The ability to safely perform subtotal excision of the gallbladder laparoscopically can decrease the rate of conversion to an open operation and potential morbidity in critically ill patients. There are several variations of subtotal cholecystectomy that can be appropriate: leaving portions of the gallbladder infundibulum, posterior wall, or both, depending on the situation. Bile leakage is not uncommon following subtotal cholecystectomy, but most bile leaks are self-limited. Those that persist have often been associated with retained common bile duct stones and have been successfully treated endoscopically. Problems with retained stones in the gallbladder remnant have not been common in reports of subtotal cholecystectomy.
Answer
D
42 When compared with standard three- or four-port laparoscopic cholecystectomy, single-incision laparoscopic surgery (SILS) is associated with which of the following?
A Lower rate of trocar site hernias
B Increased rate of bile duct injury
C Increased rate of retained common bile duct stones
D Increased rate of gallbladder perforation
E None of the above
Ref.: 18
Comments
There has been substantial interest in the development of single-incision laparoscopic approaches for many operations, including cholecystectomy, colectomy, fundoplication, and gastric band placement. Proponents of single-incision laparoscopic surgery cite the potential advantages of decreased pain and improved cosmesis in comparison with laparoscopic operations using multiple trocar sites. However, these advantages have not yet been clearly validated. So far, for most surgeons, SILS has been more difficult and time-consuming than standard laparoscopic approaches. At the time of this writing, there are no results from randomized prospective trials to judge the outcomes of SILS cholecystectomy versus standard laparoscopic cholecystectomy with multiple trocar sites.
Answer
E
43 To date, cholecystectomy using natural-orifice transluminal endoscopic surgery (NOTES) has most commonly been performed by which of the following approaches?
A Hybrid transgastric
B Hybrid transvaginal
C Hybrid transcolonic
D Pure endoscopic transvaginal
E Pure endoscopic transgastric
Ref.: 19
Comments
The worldwide experience with NOTES is increasing and it has moved into human trials. To date, the majority of procedures have involved hybrid techniques using at least one laparoscopic port in addition to the endoscopic instrumention placed via the transvaginal, transgastric, transcolonic, or transesophageal routes, depending on the operation. The largest current natural-orifice transluminal endoscopic surgery experience is with hybrid transvaginal cholecystectomy. Dedicated collaboration between teams of surgeons, endoscopists, scientists, and engineers is enabling the development of NOTES technology and investigation of relevant applications.
Answer
B
44 With regard to choledocholithiasis, which of the following statements is true?
A Common duct stones are present in one third of patients undergoing cholecystectomy.
B The incidence of common duct stones is highest in elderly patients.
C Most common duct stones are composed of calcium bilirubinate.
D Common duct stones are found more frequently when cholecystectomy is performed for chronic cholecystitis than for acute cholecystitis.
E Laparoscopic cholecystectomy is contraindicated if choledocholithiasis is suspected.
Ref.: 2, 3
Comments
About 8% to 18% of patients with symptomatic gallstones have choledocholithiasis, which has a spectrum of clinical manifestations. Approximately 6% of patients undergoing cholecystectomy have common bile duct stones that were completely unsuspected. Proper recognition of common duct stones is important because of the associated risk for biliary tract obstruction and cholangitis. The incidence of choledocholithiasis increases with each decade over the age of 60. Most common duct calculi originate in the gallbladder and are therefore of the cholesterol variety. Friable “earthy” stones (brown pigment gallstones) contain calcium complexed with bilirubinate and other anions and arise de novo in the common duct in association with biliary stasis and infection. Choledocholithiasis occurs as often with acute cholecystitis as with chronic cholecystitis. Therefore, appropriate evaluation of the patient for potential choledocholithiasis is mandatory. Laparoscopic cholecystectomy is the preferred approach for patients with choledocholithiasis. This can be accomplished in conjunction with preoperative ERCP for patients with a high likelihood of common duct stones. For those at intermediate or low risk for common duct stones, intraoperative duct imaging (cholangiography, laparoscopic ultrasound) is performed. If stones are found in the common duct, most can then be cleared with laparoscopic techniques.
Answer
B
45 Which of the following is the best indication for preoperative ERCP in a patient with gallstones?
A Obstructive jaundice
B Gallstone pancreatitis
C History of jaundice
D Alkaline phosphatase levels elevated to twice the normal
E A 10-mm common bile duct seen on ultrasonography
Ref.: 20
Comments
The rationale for preoperative endoscopic retrograde cholangiopancreatography is to identify and remove common bile duct stones so that patients may subsequently undergo laparoscopic cholecystectomy and, it is hoped, avoid the potential need for an open operation or for operative treatment of the common bile duct. However, because endoscopic evaluation of the bile duct entails its own risks, it should be selected for patients at the highest risk for choledocholithiasis. Unfortunately, there are no absolute predictors of common bile duct stones. The yield of ERCP in identifying common bile duct stones is highest in patients with obstructive jaundice or clinical cholangitis or when a duct stone is actually seen on ultrasound. In all other circumstances, most patients have negative endoscopic cholangiograms, and the examination was not necessary for most of these patients. As the number of parameters suggestive of common bile duct stones increases, however, so does the likelihood of finding stones. There is no substitute for good clinical judgment in the use of preoperative ERCP. It is an unquestionably valuable tool for diagnosing and removing common bile duct stones, but its overuse is dangerous and must be discouraged. Magnetic resonance cholangiopancreatography can be a useful noninvasive screening tool for choledocholithiasis that allows ERCP to be reserved for those with positive studies.
Answer
A
46 An intraoperative cholangiogram obtained during laparoscopic cholecystectomy shows several 2- to 3-mm filling defects in the distal common duct. What should be done next?
A Complete the laparoscopic cholecystectomy and perform ERCP postoperatively.
B Perform open surgical common bile duct exploration.
C Administer glucagon and flush the common bile duct through the cystic duct.
D Laparoscopically dilate the cystic duct and perform transcystic choledochoscopy.
E Perform laparoscopic choledochotomy.
Ref.: 21
Comments
Choledocholithiasis discovered intraoperatively can often be managed laparoscopically, depending on a number of considerations, such as the size, number, and location of the stones and the size and anatomy of the bile ducts. When approaching common bile stones laparoscopically, one should start with simple techniques and progress to more complex maneuvers as necessary. Small stones can often be cleared by flushing the common duct through a transcystic catheter after glucagon has been administered to relax the choledochoduodenal sphincter. Other transcystic manipulations can be used if the cystic duct is dilated or dilatable (with hydrostatic balloons) and provided that there is a relatively direct course between the cystic duct and the common bile duct. Such techniques include retrieval with balloon catheters or stone baskets under fluoroscopic or choledochoscopic visualization. Experienced laparoscopic surgeons can perform choledochotomy when the common bile duct is sufficiently large and simpler efforts have failed. In general, the surgeon should not leave common duct stones untreated but may elect to terminate the procedure when (1) the stones are very small or questionable, (2) the common bile duct is narrow, (3) laparoscopic clearance is not feasible, and (4) the morbidity of an open common bile duct exploration is judged to be too high for a particular patient. Intraoperative endoscopic retrieval of common bile duct stones has been successful but may be logistically impractical. Relying on postoperative endoscopy for intentionally neglected stones carries the risk that endoscopic removal may fail. A traditional open common bile duct exploration is a safe, reliable fallback for most patients when laparoscopic methods are unsuccessful and the duct is not too small.
Answer
C
47 When compared with IOC, laparoscopic ultrasound for evaluation of the common bile duct during cholecystectomy is most associated with each of the following except:
A Better sensitivity for detecting common duct stones
B Less time requirement
C Increased risk for common bile duct injury
D Less accurate identification of the proximal bile ducts
E Better identification of vascular variations
Ref.: 22
Comments
Intraoperative cholangiography and intraoperative ultrasonography are the most commonly used methods for evaluating the bile ducts during cholecystectomy. Some of the advantages of sonography are that it is relatively quick, it can be performed without the need for dissection of the cystic duct, and it can easily be repeated. Intraoperative ultrasound is more sensitive than IOC for the detection of small stones or sludge in the common bile duct, although these findings may not necessarily be clinically relevant. Sonography can also demonstrate the vascular anatomy of the hepatoduodenal region. Ultrasound is less reliable than cholangiography for delineation of the anatomy of the proximal bile ducts, such as the presence of separately inserting segmental hepatic ducts. Both imaging methods can be useful in the avoidance of bile duct injury.
Answer
C
48 Which of the following is the best treatment for a patient with choledocholithiasis 3 years after cholecystectomy?
A Administration of ursodeoxycholic acid
B Percutaneous transhepatic stone extraction
C Endoscopic sphincterotomy and stone extraction
D Common bile duct exploration and T-tube placement
E Common bile duct exploration and choledochoduodenostomy
Ref.: 2, 3
Comments
Most common bile duct stones found in patients after cholecystectomy can be treated successfully by nonoperative methods. Stone extraction through a T tube or endoscopically after endoscopic sphincterotomy if the patient does not have a T tube in place results in successful duct clearance with a low complication rate in more than 90% of patients. By definition, bile duct stones occurring more than 2 years after cholecystectomy are considered primary common duct stones. These are pigment gallstones related to biliary stasis and infection rather than the typical cholesterol stones found in the gallbladder. In addition to stone removal, some type of ductal drainage procedure is therefore also indicated in most of these patients to prevent stone recurrence.
When performed by experienced clinicians, endoscopic sphincterotomy is successful in more than 90% of patients and, when combined with endoscopic extraction with the use of balloon catheters or baskets, results in stone clearance in 85% to 90% of patients. Duct stones have been removed successfully via the percutaneous transhepatic route when endoscopic approaches are not successful.
A number of situations may make endoscopic clearance of bile duct stones difficult or unsuccessful, including large impacted stones, the presence of a distal bile duct stricture, previous gastrectomy with gastroenterostomy or Roux-en-Y anastomosis, complications of endoscopic sphincterotomy before stone extraction, or the presence of a duodenal diverticulum. If access to the bile duct can be achieved endoscopically, adjuvant modalities, such as intracorporeal fragmentation techniques (i.e., mechanical, electrohydraulic, or laser lithotripsy) or ESWL, may allow successful removal of even difficult stones. Reoperation on the biliary tract for clearance of duct stones is reserved for physiologically fit patients in whom other extraction techniques are unsuccessful. Ursodeoxycholic acid does not dissolve pigment stones.
Answer
C
49 Which of the following is the most appropriate initial test for the evaluation of obstructive jaundice?
A HIDA scan
B Ultrasound imaging
C CT
D PTC
E ERCP
Ref.: 2, 3
Comments
All of the aforementioned imaging modalities may be useful for evaluating a patient with obstructive jaundice. Overall, ultrasound is the most cost-effective initial examination. It permits identification or visualization of ductal dilation, suggests the level of obstruction, and provides information about the liver, the pancreas, and the presence or absence of calculous disease. CT or magnetic resonance imaging may best delineate the anatomy of mass lesions in the hepatobiliary and pancreatic region and assist in the preoperative assessment of resectability. Magnetic resonance cholangiography can provide precise delineation of ductal anatomy and is increasingly important in the evaluation of malignant disease. Percutaneous transhepatic cholangiography can demonstrate the proximal extent of obstruction and is useful for assessing the suitability of the proximal hepatic ducts for anastomosis. Endoscopic retrograde cholangiopancreatography is particularly useful in cases of distal biliary tract obstruction and allows evaluation of the ampullary region. Both PTC and ERCP allow cytologic or histologic sampling, and both can be used to place catheters for decompression of the obstructed biliary tract. Although 99mTc-iminodiacetic acid scans can demonstrate ductal obstruction, they do not provide sufficient anatomic definition to determine cause or assist in making therapeutic decisions.
Answer
B
50 Two weeks following hepaticojejunostomy for the treatment of a benign bile duct stricture, a patient has a serum bilirubin level of 6 mg/dL. The patient was jaundiced for 4 weeks before the operation and had a preoperative serum bilirubin level of 12 mg/dL. Which of the following is the most likely explanation for this current serum bilirubin level?
A Anastomotic stricture
B Persistent delta-bilirubinemia
C Postoperative hepatitis
D Normal expected decline after relief of any obstructive jaundice
E Renal failure
Ref.: 4
Comments
After relief of biliary obstruction, there is a prompt increase in bile flow, and normal bile acid secretion resumes within several days. Serum bilirubin levels decline approximately 50% by 36 to 48 hours after surgery and 8% per day thereafter. This rate varies, depending on the duration of the jaundice. Delta-bilirubin is a form of bilirubin that is covalently bonded to albumin and is measured as part of the direct bilirubin fraction. As such, it is not filtered by the kidneys and has the same serum half-life as albumin, approximately 18 days, which accounts for the slow decline in serum bilirubin levels observed in patients following relief of long-standing jaundice. Although 90% of patients who had jaundice for 1 week or less have a normal serum bilirubin level 3 to 4 weeks postoperatively, only one third of patients who had jaundice for 4 weeks or longer obtain normal levels by the same time. Anastomotic stenosis does not usually develop early during the postoperative period. Postoperative hepatocellular dysfunction as a result of hepatitis or other causes can occur early in the postoperative period, but it is a less likely cause of hyperbilirubinemia in a patient whose serum bilirubin levels are gradually declining and who would be anticipated to have persistent delta-bilirubinemia.
Answer
B
51 Which of the following is the most likely explanation for a serum bilirubin level of 40 mg/dL in a patient with obstructive jaundice?
A The patient has complete biliary obstruction.
B The duration of obstruction has exceeded 2 weeks.
C The patient has associated renal dysfunction.
D The patient has malignant biliary obstruction.
E The patient also has Gilbert disease
Ref.: 4
Comments
In the presence of complete biliary obstruction, serum bilirubin levels generally plateau at 25 to 30 mg/dL. At this point, the daily bilirubin load equals that excreted by the kidneys. Situations in which even higher bilirubin levels can be found include renal insufficiency, hemolysis, hepatocellular disease, and rarely, a bile duct–hepatic vein fistula. Hyperbilirubinemia tends to be more pronounced in patients with obstruction caused by malignant disease than with obstruction resulting from benign causes. However, malignant obstruction in the absence of the previously enumerated factors does not produce this degree of hyperbilirubinemia.
Answer
C
52 The pathophysiology of acute renal failure in a patient with biliary obstruction is related to which of the following conditions?
A Renal hypertension
B Hyperbilirubinemia
C Hepatorenal syndrome
D Bile acidemia
E Acute glomerulonephritis
Ref.: 4
Comments
Acute renal failure is a frequent and commonly fatal complication of biliary sepsis. A number of factors contribute to the development of this complication. Renal hypoperfusion occurs as a result of bacteremia, systemic hypotension, and hypovolemia. Circulating bacterial endotoxins are also nephrotoxic. Patients with biliary obstruction are at higher risk for renal failure than are patients with sepsis from other causes. Evidence suggests that circulating bile acids themselves may induce tubular damage and exacerbate the effects of renal ischemia. Therapy for patients with biliary sepsis must focus on adequate fluid and vasopressor support, antibiotic coverage, and biliary decompression to prevent renal failure. Additional treatment, such as the administration of bile acids to minimize gut absorption of bacterial endotoxins, has also been used. Little evidence exists to indicate that renal damage is caused by bilirubin, even though it may predispose the tubular cells to ischemia.
Answer
D
53 Which of the following conditions is usually associated with the highest incidence of positive bile culture results?
A Acute cholecystitis
B Chronic cholecystitis
C Choledocholithiasis
D Postoperative bile duct stricture
E Bile duct malignancy
Ref.: 2, 4
Comments
Recognition of clinical situations in which bacteria are likely to be present in bile is important because the presence of bacteria in bile is correlated with the risk for postoperative infectious complications. Prophylactic antibiotics have decreased infectious morbidity in patients older than 50 years and in those with jaundice, acute cholecystitis, or choledocholithiasis and cholangitis. Bile cultures are positive in approximately 5% to 40% of patients with chronic cholecystitis, 30% to 70% of patients with acute cholecystitis, 60% to 80% of patients with choledocholithiasis, and nearly all patients with bile duct stricture. Bacterial infection of bile occurs in 25% to 50% of patients with malignant obstruction. Bile culture results are expected to be positive in any patient with an indwelling biliary tube.
Answer
D
54 Which of the following organisms is most commonly isolated from bile?
A Escherichia coli
B Clostridium spp.
C Bacteroides fragilis
D Pseudomonas spp.
E Enterococcus spp.
Ref.: 2, 4, 7
Comments
All of the aforementioned organisms are found in the biliary tract, but gram-negative aerobic organisms, particularly E. coli and Klebsiella, are found most frequently. Other gram-negative aerobic bacteria that can be cultured are Proteus, Pseudomonas, and Enterobacter spp. Gram-positive organisms, especially Enterococcus spp. and Streptococcus faecalis, are also frequently observed. Anaerobes are now recognized in 25% to 30% of cases, most commonly B. fragilis, followed by Clostridium spp. Polymicrobial infection occurs in approximately 60% of cases. Prophylactic or therapeutic antibiotic therapy must be effective against the anticipated organisms. Severe biliary sepsis is usually treated with broad-spectrum or combination antibiotics that are effective against gram-negative organisms, anaerobes, and enterococci.
Answer
A
55 Which of the following is the most common mechanism leading to bacteria in bile?
A Ascending infection from the duodenum
B Hematogenous portal venous spread
C Hematogenous arterial spread
D Lymphatic spread
E Systemic immunosuppression
Ref.: 2, 4
Comments
Bile is usually sterile. There are various routes by which bacteria can reach the biliary tract, and although not proved, dissemination from the portal venous system via the liver is favored as the most common mechanism. Ascending infection from the duodenum does not occur to a significant extent. In addition, evidence suggests that the direction of lymphatic flow is from the liver downward rather than in the reverse direction. Hematogenous dissemination via hepatic arterial flow is a mechanism of hepatic abscess formation and may lead to bactibilia but is thought to be less common than portal venous spread.
Answer
B
56 Which of the following conditions is sufficient to cause cholangitis with bacteremia?
A Bacteria in bile
B Partial bile duct obstruction
C Complete bile duct obstruction
D Any of the above
E None of the above
Ref.: 2, 7
Comments
The pathophysiology of cholangitis requires both bacterial infection of bile and bile duct obstruction with elevated intraductal pressure. Neither the presence of bacteria in bile nor biliary obstruction alone is sufficient to produce bacteremia. When bacteria are present in bile and common duct pressures exceed 20 cm H2O, cholangiovenous and cholangiolymphatic reflux occurs and results in systemic bacteremia. Partial or complete bile duct obstruction may produce cholangitis if bacteria are present. In fact, cholangitis occurs more commonly with partial obstruction because it is more frequently associated with stone disease, whereas complete obstruction is more often found with malignancy. Calculous disease is the most common cause of cholangitis, which is understandable because it is associated with both bile duct obstruction and bacterial infection.
Answer
E
57 If an antibiotic is effective against the bacteria present in bile, which of the following is the most important consideration for effective treatment of biliary tract infection?
A Serum concentration of the antibiotic
B Bile concentration of the antibiotic in an unobstructed biliary tract
C Bile concentration of the antibiotic in an obstructed biliary tract
D Potential renal toxicity of the antibiotic
E Hospital Surgical Care Improvement Project (SCIP) guidelines
Ref.: 2, 4
Comments
The most important pharmacologic considerations pertaining to selection of antimicrobial agents for the treatment of biliary sepsis are the spectrum of antibacterial activity of the agent and achievement of adequate serum levels of the drug. Therapy cannot be adequate if the agents selected are not effective against the anticipated organisms (i.e., gram-negative Enterobacteriaceae, enterococci, and anaerobes) or if dosing does not produce sufficient serum levels. The significance of biliary levels of antibiotics is often discussed, but they are of little clinical importance. High bile levels of an antibiotic are meaningless if the agent is not effective against the bacteria present. Moreover, agents that achieve high concentrations in the normal biliary tract may not reach such levels in the presence of biliary obstruction. The aminoglycoside gentamicin, for example, has traditionally been an effective agent against the gram-negative organisms that cause biliary sepsis, but it is not concentrated in bile. The potential nephrotoxicity of an antibiotic is an important consideration because the risk for renal compromise already exists in a patient with sepsis and biliary obstruction. This has encouraged the use of nonaminoglycoside drugs for gram-negative coverage, but this consideration is not as important as the activity spectrum and adequate serum levels of the drugs.
Answer
A
58 In addition to fluid resuscitation and intravenous antibiotics, most patients with acute cholangitis require urgent treatment with which of the following?
A Laparoscopic cholecystectomy
B Percutaneous transhepatic drainage
C Endoscopic sphincterotomy and drainage
D T-tube decompression of the common bile duct
E None of the above
Ref.: 2, 7
Comments
Charcot’s triad, which consists of fever, jaundice, and upper abdominal pain, is the clinical hallmark of acute cholangitis. When accompanied by shock and changes in mental status, it is referred to as Reynold’s pentad. Cholangitis varies widely in severity, and treatment must be individualized according to the patient’s condition. Initial therapy consists of fluid resuscitation and antibiotics that are effective against gram-negative organisms, enterococci, and anaerobes. Approximately 5% to 10% of patients initially have severe toxic cholangitis and manifestations of the Reynold pentad. Patients who fail to improve or who deteriorate despite antibiotic and fluid support require urgent biliary decompression. This can generally be accomplished nonoperatively by percutaneous transhepatic or endoscopic approaches, depending on the suspected location of the obstruction based on ultrasonographic findings and on the availability of local expertise in these procedures. The ability to decompress the biliary tract nonoperatively in these cases has been advantageous because it not only allows stabilization of a high percentage of patients but also permits diagnostic cholangiography to be performed when the patient has stabilized. When initial operative decompression of the biliary tract was the only approach for these critically ill patients, the mortality rate was high, and there was a frequent need for subsequent reoperation on the biliary tract because of the inability to identify or deal with the underlying pathologic condition at the time of the initial operation. If effective nonoperative drainage of the biliary tract is not possible, surgery should not be delayed in these critically ill patients. T-tube decompression of the common bile duct is performed. Choledochoduodenostomy is not performed in critically ill patients, but it can be considered if the common bile duct is dilated to 15 mm or greater, the patient is physiologically stable, and other conditions permit safe performance of an anastomosis. The current mortality rate in patients with acute cholangitis is approximately 5%. Poor prognostic factors include renal failure, liver abscess, cirrhosis, and proximal malignant obstruction.
Answer
E
59 Ultrasound of the gallbladder demonstrates a 5-mm hyperechoic focus along the gallbladder wall that does not move or produce shadowing and that has a “comet tail” echo pattern behind it. What is the most likely diagnosis?
A Adenomatous polyp
B Cholesterol polyp
C Gallstone
D Adenomyomatosis
E Xanthogranulomatous inflammation
Ref.: 6
Comments
The term hyperplastic cholecystosis describes a group of benign proliferative conditions of the gallbladder, including cholesterolosis and adenomyomatosis, or adenomatous hyperplasia. These conditions can be symptomatic and are often diagnosed on the basis of their sonographic features. Cholesterolosis consists of deposits of cholesterol in foamy histiocytes in the gallbladder wall. A localized collection of such cholesterol-laden cells covered by a normal layer of epithelium and connected to the mucosa by a small pedicle is known as a cholesterol polyp. Ultrasound imaging shows hyperechoic foci with a “comet tail” artifact. Unlike gallstones, the foci do not move or produce acoustic shadowing. Adenomatous hyperplasia is a proliferative lesion characterized by increased thickness of the mucosa and muscle along with mucosal diverticula known as Rokitansky-Aschoff sinuses. Segmental, diffuse, and localized forms of adenomyomatous hyperplasia have been described. Of these, a localized form involving the fundus of the gallbladder is most frequently encountered. Ultrasound demonstrates a mass lesion or “pseudotumor.” Adenomatous polyps are true neoplasms derived from the glandular epithelium of the gallbladder. Xanthogranulomatous inflammation is a condition in which foamy histiocytes are found in conjunction with inflammatory cells and a fibroblastic vascular reaction, often with mucosal ulceration.
Answer
B
60 With regard to adenomyomatosis of the gallbladder, which of the following statements is true?
A It is a premalignant lesion.
B It results from chronic inflammation.
C It may cause right upper quadrant pain in the absence of gallstones.
D It is rarely associated with cholelithiasis and cholecystitis.
E It is not an indication for cholecystectomy in asymptomatic patients.
Ref.: 1, 2
Comments
Adenomyomatosis is a hyperplastic abnormality of the gallbladder that is not related to inflammation or neoplasia. Approximately one half or more of patients with adenomyomatosis also have cholelithiasis and cholecystitis, but the relationship is not causal. Adenomyomatosis is not a premalignant lesion. The hyperplastic conditions of adenomyomatosis and cholesterolosis may be associated with functional abnormalities of the gallbladder, as evidenced by disturbances in motility or hyperconcentration during oral cholecystography. These abnormalities may be the cause of biliary tract symptoms in patients with hyperplastic cholecystosis in the absence of cholelithiasis. Cholecystectomy can relieve the symptoms in these patients.
Answer
C
61 Which of the following is the most common type of biliary enteric fistula?
A Cholecystocolic
B Cholecystoduodenal
C Cholecystoduodenocolic
D Choledochoduodenal
E Choledochogastric
Ref.: 2, 4
Comments
Almost all internal biliary fistulas are acquired communications between the extrahepatic biliary tree and the intestinal tract. In rare instances, acquired or congenital bronchobiliary or acquired pleurobiliary fistulas occur. Biliary enteric fistulas most commonly involve the gallbladder and the duodenum (70% to 80% of cases) and are the result of chronic inflammation caused by gallstone disease. The second most common fistula occurs between the gallbladder and colon; infrequently, the stomach or multiple sites (cholecystoduodenocolic) are involved. Occasionally, the biliary site of the fistula is the common bile duct. Choledochoduodenal fistulas are most frequently caused by penetrating peptic ulcers, but they might occur in patients with choledocholithiasis and previous cholecystectomy. Other, less common causes of biliary enteric fistulas are malignancy and penetrating trauma.
Answer
B
62 With regard to the management of a patient with gallstone ileus, which of the following statements is true?
A Initial tube decompression and nonoperative management allow spontaneous stone passage in one third of patients.
B Operative treatment attempts to displace the stone into the colon without enterotomy.
C Operative treatment involves enterotomy proximal to the site of obstruction.
D Cholecystectomy and fistula repair at the time of stone removal are contraindicated.
E Standard treatment is initial laparotomy for stone removal and reoperation for cholecystectomy when the patient is stable.
Ref.: 2, 4
Comments
Gallstone ileus is mechanical obstruction of the gastrointestinal tract caused by a gallstone that has entered the intestine via an acquired biliary enteric fistula. Although gallstone ileus accounts for only 1% to 3% of all small bowel obstructions, it is associated with a higher mortality rate than other nonmalignant causes of bowel obstruction because it tends to occur in the elderly population and typical cases are characterized by diagnostic delay as a result of waxing and waning of symptoms (“tumbling obstruction”). Pathognomonic radiologic features include a gas pattern of small bowel obstruction with pneumobilia and an opaque stone outside the expected location of the gallbladder. Not all of these radiologic features are usually present, however. The most common site of obstruction is the terminal ileum. Infrequently, sigmoid obstruction occurs in an area narrowed by intrinsic colonic disease.
Initial therapy is appropriate resuscitation followed by surgery. Spontaneous passage is a rare phenomenon, and nonoperative management is associated with a prohibitive mortality rate. Stone removal is best accomplished with an enterotomy placed proximal to the site of obstruction. Care must be taken to search for additional intestinal stones, which are present in 10% of patients. Attempts to crush the stone extraluminally or to milk it distally are contraindicated because they may cause bowel injury. In rare instances, small bowel resection is necessary if there is ischemic compromise or bleeding at the site of impaction.
The main controversy regarding surgical treatment of gallstone ileus is whether a definitive biliary tract operation with cholecystectomy, fistula repair, and possible common duct exploration should be performed at the time of stone removal. This decision must be based on sound surgical judgment and consideration of the underlying physiologic status of the patient and the anatomic status of the right upper quadrant. Up to one third of patients who do not undergo definitive biliary surgery experience recurrent biliary symptoms, including cholecystitis, cholangitis, and recurrent gallstone ileus. Furthermore, the rate of spontaneous fistula closure is open to question. For these reasons, a definitive one-stage procedure should be considered in physiologically fit patients if right upper quadrant dissection does not prove unduly hazardous from a technical standpoint, particularly if residual stones can be demonstrated in the right upper quadrant. In properly selected patients, a definitive one-stage procedure is not associated with higher operative morbidity or mortality rates. However, because most of these patients are elderly and have a high incidence of comorbid disease, surgical therapy has been limited to stone removal in most instances. Interval cholecystectomy should be considered for patients with postoperative biliary symptoms and for those with residual right upper quadrant stones, provided that they are physiologically fit. In reality, because of the compromised underlying status of many of these patients, interval elective procedures are not commonly performed.
Answer
C
63 Which of the following is the preferred management of a type I choledochal cyst?
A Cyst excision
B Cyst duodenostomy
C Cyst jejunostomy
D External drainage
E Endoscopic sphincterotomy
Ref.: 2
Comments
Cystic disease of the biliary tract may involve the intrahepatic ducts, extrahepatic ducts, or both. The most common form of involvement is cystic dilation of the extrahepatic bile duct (type I). Combined intrahepatic and extrahepatic cysts (type IV) are next in frequency of occurrence. A diverticulum of the common bile duct (type II), a “choledochocele” extending from the distal duct into the duodenum (type III), and cystic disease confined to the intrahepatic ducts (type V) are less common. Bile duct cysts may be associated with jaundice, abdominal pain, and cholangitis in both adult and pediatric patients. Furthermore, their association with biliary tract malignancy and with anomalous relationships between the pancreatic duct and bile duct is well recognized. For these reasons, complete cyst excision with Roux-en-Y hepaticojejunostomy is the preferred treatment. Internal drainage procedures are followed by a high rate of recurrent jaundice, cholangitis, and stricture. In some instances, because of the intrahepatic or retroduodenal extent of disease or because of technical considerations, complete excision may not be feasible, and the surgeon may have to settle for partial excision. Endoscopic treatment by sphincterotomy or resection is occasionally appropriate for the rarely occurring choledochocele.
Answer
A
64 With regard to balloon dilation of benign biliary strictures, which of the following statements is true?
A Dilation can be performed via the transhepatic or endoscopic route.
B Repeated dilations are not often required.
C Perforation of the bile duct is the most frequent complication.
D Better success is obtained with anastomotic strictures than with primary duct strictures.
E The long-term success rate is better than that achieved with surgical repair.
Ref.: 2, 3
Comments
Nonoperative dilation of benign biliary strictures via endoscopic or percutaneous transhepatic access is an alternative to surgery that may be appropriate for some patients. Repeated dilations are often required, but overall success rates of 70% to 80% at 2 to 3 years of follow-up have been reported. Success has generally been somewhat higher in patients with primary ductal strictures than in those with strictures of biliary enteric anastomoses. Bleeding and sepsis have been the most frequent complications and can be life-threatening. Data on long-term results are limited. Comparison between balloon dilation and surgery has demonstrated better long-term results (approximate mean follow-up at 5 years) with surgery, but no difference in overall morbidity, hospitalization, or cost between the two therapies. It cannot be ensured that the treatment groups are comparable, however. Nonoperative dilation of biliary strictures may be appropriate as initial treatment of a strictured biliary anastomosis or for patients in whom surgical repair is deemed excessively difficult or dangerous. The decision about how a biliary stricture is initially treated and when nonoperative maneuvers are abandoned in favor of surgery should be made in consultation with a skilled endoscopist, an interventional radiologist, and an experienced hepatobiliary surgeon.
Answer
A
65 A 40-year-old man is evaluated for fluctuating jaundice, pruritus, and fatigue. Liver enzyme levels demonstrate cholestasis. Ultrasound imaging does not show gallstones or bile duct dilation. What diagnostic test should be obtained next?
A Measurement of serum antimitochondrial antibodies
B CT
C HIDA scan
D ERCP
E Liver biopsy
Ref.: 2-4
Comments
The findings described are fairly typical of sclerosing cholangitis, which can also be discovered in asymptomatic patients based on a cholestatic liver enzyme pattern. Sclerosing cholangitis is a disease of undetermined cause characterized by inflammatory fibrosis and stenosis of the bile ducts. The process can be considered primary when no specific etiologic factor is identified or secondary when associated with specific causes, such as bile duct stones, operative trauma, hepatic arterial infusion of chemotherapeutic agents, or intraductal instillation of various irritants for the treatment of echinococcal disease. Primary sclerosing cholangitis may be an isolated finding or may occur in conjunction with a variety of other disease processes, most commonly ulcerative colitis and pancreatitis. Although the cause of primary sclerosing cholangitis is unknown, most attention has focused on an autoimmune or infectious cause. Evidence of an autoimmune cause is largely inferential and based on the association of sclerosing cholangitis with a variety of autoimmune diseases. Abnormal immunologic parameters can be found in the serum of some patients with sclerosing cholangitis, but there are no specific serologic markers for the disease. Antimitochondrial antibodies are generally associated with primary biliary cirrhosis. The diagnosis is usually made following ERCP showing multiple strictures and dilations, which give a “beaded” appearance to the ducts. Magnetic resonance imaging of the bile ducts may also show abnormalities. Typically, sclerosing cholangitis is a diffuse process that affects both the intrahepatic and extrahepatic bile ducts. In some cases, more limited involvement of the distal bile duct, the intrahepatic ducts, or the area of the bifurcation can be seen. Liver biopsy may show fibro-obliterative cholangitis or cirrhosis as the disease progresses.
Answer
D
66 Definitive treatment of a patient with sclerosing cholangitis and biliary cirrhosis involves which of the following?
A Ursodeoxycholic acid
B Corticosteroids
C Endoscopic balloon dilation and stenting
D Extrahepatic bile duct resection and transhepatic stenting
E Hepatic transplantation
Ref.: 2-4
Comments
Once sclerosing cholangitis has progressed to cirrhosis, the only definitive treatment is hepatic transplantation. The results of transplantation are generally similar to those obtained when it is performed for other indications. Before the development of cirrhosis, a number of medical and surgical therapies may be useful. Pharmacologic approaches have included the use of immunosuppressants, bile acid–binding agents, and antifibrotic and antimicrobial drugs. Unfortunately, there is little evidence that any medical therapy has been effective in slowing progression. Some hopeful results have been reported with ursodeoxycholic acid, which may improve liver enzyme test results and liver histologic study results. Dominant strictures can be treated operatively or by nonoperative dilation via endoscopic or percutaneous transhepatic approaches. The long-term efficacy of nonoperative approaches has often been limited, however. Select patients with predominantly extrahepatic or bifurcation strictures have been treated successfully with bile duct resection followed by Roux-en-Y reconstruction and long-term anastomotic stenting.
Answer
E
67 Following cholecystectomy, an adenocarcinoma of the gallbladder extending into the subserosa is discovered incidentally. The recommended treatment includes which of the following?
A Nothing further at this time
B External beam radiation therapy
C Radiation therapy and chemotherapy
D Reoperation for liver resection and lymphadenectomy
E Reoperation for performance of pancreaticoduodenectomy
Ref.: 22
Comments
When gallbladder cancer is discovered postoperatively during pathologic examination of the specimen, the depth of tumor invasion is an important determinant of further therapy. Tumors limited to the mucosa (T1a) are usually cured by cholecystectomy alone. Patients with tumors extending into the muscle layer (T1b) or into the subserosal connective tissue layer (T2) are those most likely to benefit from resection of the adjacent liver segments (IV and V) and hepatoduodenal lymphadenectomy. A substantial proportion of patients with T2 lesions can be found to have lymph nodes positive for cancer or residual disease. Reoperation may increase the 5-year survival rate to 70% to 90% as compared with 40% for cholecystectomy alone. More extensive invasion through the serosa (T3) or more than 2 cm into the liver (T4), with or without invasion of adjacent organs, may be recognized by the surgeon at the time of cholecystectomy, but such is not always the case. Cholecystectomy is inadequate for cure of these lesions. Radical resection of these cancers may certainly benefit some patients, but the morbidity and mortality may be high, and conclusive evidence of benefit to many patients is lacking. Other pathologic findings in the gallbladder specimen that favor reoperation are a cancer-positive cystic duct margin (in which case bile duct resection must be considered) or a cancer-positive cystic duct lymph node. Radiation therapy and chemotherapy have generally been ineffective for the treatment of gallbladder cancer.
Answer
D
68 Ultrasound imaging demonstrates a 15-mm polypoid lesion in the gallbladder of an asymptomatic 60-year-old patient. Which of the following best describes the recommended treatment?
A Observation with repeated ultrasound studies in 6 months
B Cholecystectomy
C Cholecystectomy if the patient is female
D Cholecystectomy only if symptoms develop
E Cholecystectomy only if the patient also has gallstones
Ref.: 23
Comments
Polypoid lesions of the gallbladder may be benign, premalignant, or malignant. Inflammatory polyps and cholesterol polyps are benign, nonneoplastic lesions. Benign adenomas are neoplasms that have a malignant potential similar to that of adenomas arising in other areas of the gastrointestinal tract. Polypoid lesions are typically diagnosed by ultrasound imaging and occasionally by other imaging modalities, such as CT. The indications for cholecystectomy for the treatment of a polypoid lesion are (1) symptoms and (2) possible malignancy.
The risk for malignancy is related to the size of the lesion; it is higher for lesions that are 10 mm or larger and is quite substantial for lesions measuring 15 mm. Therefore, cholecystectomy is performed if the patient has biliary tract symptoms—regardless of polyp size or the presence or absence of gallstones—or if the lesion is larger than 10 mm. Polypoid lesions in patients 60 years or older are also more frequently malignant. The use of laparoscopic cholecystectomy for polypoid lesions is controversial. Proponents argue that the laparoscopic approach is appropriate, because most polyps are benign and even limited cancers may be cured by cholecystectomy alone. However, gallbladder leakage is not infrequent during laparoscopic cholecystectomy, and consequent dissemination of otherwise “curable” early cancers has been reported. It is generally advised that “open cholecystectomy” be performed for patients considered at risk for gallbladder cancer.
Answer
B
69 Which of the following is a contraindication to resection of an adenocarcinoma of the bile duct?
A Tumor location in the distal common bile duct
B Tumor location at the bifurcation of the bile duct
C Peritoneal metastases
D Invasion of the right portal vein and right hepatic artery
E None of the above
Ref.: 3, 4
Comments
Cancers of the extrahepatic bile ducts usually carry a poor prognosis because these tumors are frequently beyond the confines of surgical resection at the time of diagnosis. Substantial palliation can often be achieved with therapy directed at the relief of biliary obstruction. The prognosis is related to tumor location, resectability, and histologic pattern. Proximal lesions at or near the hepatic bifurcation are most common but are also least often resectable and therefore have a less favorable prognosis. Aggressive resection of proximal lesions, usually including hepatic resection, can improve survival. Hilar cholangiocarcinoma (Klatskin tumor) is considered unresectable if there is metastatic disease, bilateral involvement of the portal vein or hepatic artery, or bilateral extension of the tumor to second-order biliary radicles. Hepatic transplantation for otherwise unresectable tumors has had poor results. Distal lesions resectable by pancreaticoduodenectomy have the best prognosis, with a 5-year survival rate of approximately 30%. Palliative decompression can be achieved by surgical anastomosis, surgical intubation, or endoscopic or percutaneous catheter placement. The most appropriate method of palliative decompression for a particular patient depends on tumor location and extent, the patient’s underlying condition, the expertise of the surgeon, and the anticipated complications associated with each technique. Nonoperative decompression is preferred for patients who are demonstrated to have metastasis or otherwise unresectable disease before surgery.
Answer
C
70 How is a contusion of the gallbladder from blunt abdominal trauma best managed?
A Observation
B Placement of a percutaneous cholecystostomy tube
C Placement of an endoscopic biliary stent
D Suture imbrication of the contusion
E Cholecystectomy
Ref.: 2
Comments
The gallbladder may be injured as a result of blunt or penetrating trauma. Penetrating injury is the most common. Most injuries of the gallbladder and extrahepatic biliary tree are associated with involvement of other organs, such as the liver, small bowel, and colon. Blunt injuries, including contusion, avulsion, and rupture, are treated by cholecystectomy. Penetrating injuries occasionally cause isolated injury to the gallbladder. Treatment in such instances is usually cholecystectomy, although cholecystostomy or simple closure plus drainage is conceivable. The prognosis following a nonoperative injury to the biliary tract is related to the significance of the associated injuries.
Answer
E
References
1 Deziel DJ. The journey of the surgeon-hero. Surg Endosc. 2008;22:1-7.
2 Chari RS, Shah SA. Biliary system. In Townsend CM, Beauchamp RD, Evers BM, et al, editors: Sabiston textbook of surgery: the biological basis of modern surgical practice, ed 18, Philadelphia: WB Saunders, 2008.
3 . Hepatobiliary and Portal Venous System Section. Mullholland MW, Lillemoe KD, Doherty GM, et al, editors. ed 4. Lippincott Williams & Wilkins, Philadelphia, 2006.
4 Blumgart LH. Surgery of the liver, biliary tract and pancreas, ed 4. Edinburgh: Churchill-Livingstone; 2006.
5 Yoshida J, Chijiwa K, Yamaguchi K, et al. Practical classification of the branching types of the biliary tree: an analysis of 1,094 consecutive direct cholangiograms. J Am Coll Surg. 1996;82:37-40.
6 Machi J, Staren ED. Ultrasound for surgeons. Philadelphia: Lippincott Williams & Wilkins; 2005.
7 Mulvihill SJ. Liver, biliary tract, and pancreas. In O’Leary JP, Tabuenca A, editors: The physiologic basis of surgery, ed 4, Philadelphia: Lippincott Williams & Wilkins, 2008.
8 Canfield AJ, Hetz SP, Schriver JP, et al. Biliary dyskinesia: a study of more than 200 patients and review of the literature. J Gastrointest Surg. 1998;2:443-448.
9 Fong Y, Brennan MF, Turnbulla A, et al. Gallbladder cancer discovered during laparoscopic surgery. Arch Surg. 1993;128:1050-1054.
10 Strasberg SM, Hertle M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101-125.
11 Lillemoe KD. Current management of bile duct injury. Br J Surg. 2008;95:403-405.
12 Deziel DJ. Complications of cholecystectomy. Surg Clin North Am. 1994;74:809-823.
13 Stewart L, Way LW. Bile duct injuries during laparoscopic cholecystectomy: factors that influence the results of treatment. Arch Surg. 1995;130:1123-1129.
14 Lillemoe KD, Martin SA, Cameron JL, et al. Major bile duct injuries during laparoscopic cholecystectomy. Ann Surg. 1997;225:459-471.
15 Woods MS, Traverso LW, Kozarek RA, et al. Biliary tract complications of laparoscopic cholecystectomy are detected more frequently with routine intraoperative cholangiography. Surg Endosc. 1995;9:1076-1080.
16 Date RS, Kaushal M, Ramesh A. A review of the management of gallstone disease and its complications during pregnancy. Am J Surg. 2008;196:599-608.
17 Palanivelu C, Rajan PS, Jani K, et al. Laparoscopic cholecystectomy in cirrhotic patients: the role of subtotal cholecystectomy and its variants. J Am Coll Surg. 2006;203:145-151.
18 Podolsky ER, Curcillo PGII. Single port access (SPA) surgery: a 24-month experience. J Gastrointest Surg. 2010;14:759-767.
19 Horgan S, Mintz Y, Jacobsen GR, et al. NOTES: transvaginal cholecystectomy with assisting articulating instruments. Surg Endosc. 2009;23:1900.
20 Barkun AN, Barkun JS, Fried GM, et al. Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. Ann Surg. 1994;220:32-39.
21 Petelin J. Laparoscopic approach to common duct pathology. Am J Surg. 1993;165:487-491.
22 Perry KA, Myers JA, Deziel DJ. Laparoscopic ultrasound as the primary modality for bile duct imaging during cholecystectomy. Surg Endosc. 2008;22:208-213.
23 D’Angelica M, Dalal KM, DeMatteo RP, et al. Analysis of the extent of resection for adenocarcinoma of the gallbladder. Ann Surg Oncol. 2009;16:806-816.