Timothy J. Fortuna and John H. Burton
Expertise in airway management is an essential skill for the emergency physician (EP), and this is especially true of airway management in patients with multisystem trauma. Many trauma patients benefit from early control of the airway to ensure adequate oxygenation and ventilation and to protect against aspiration.
There are many special considerations to take into account when faced with controlling and maintaining an adequate airway in the trauma patient; some are listed in Table 19.1. The EP should assume the presence of cervical spine injury in most victims of blunt trauma. Owing to the common occurrence of altered mental status and hemodynamic instability, as well as the difficulty of rapidly obtaining adequate cervical spine imaging, cervical spine injury cannot typically be excluded in many trauma patients who require emergent intubation.
TABLE 19.1
Factors Complicating Trauma Airway Management
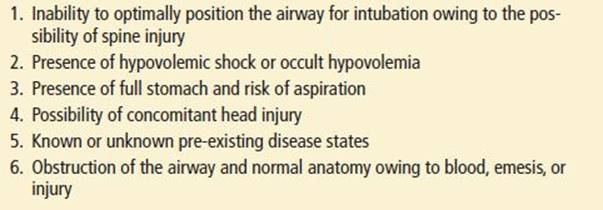
There are many methods for predicting the difficulty of intubation in a patient (see Chapter 1). Though these are helpful as a structured approach to airway management, their application in the trauma patient is frequently limited. Coexisting facial and penetrating neck trauma may exacerbate the challenge of both the assessment and visualization of the airway. The inability to optimally position the airway in the trauma patient can be problematic for adequate laryngeal visualization during intubation.
All trauma patients should be assumed to have hypovolemia or compensated shock. Therefore, caution must be used when choosing medications to facilitate airway management to avoid hemodynamic compromise. Trauma patients should also be presumed to have a full stomach. This places the trauma patient at an elevated risk for aspiration during the initial assessment and airway interventions. Patients immobilized by cervical collar and long spine board are not always able to fully protect their airways.
Concomitant head injury alters the approach to airway management in the trauma patient. Adequate cerebral perfusion pressure should be maintained in these patients and the consequence of potentially increased intracranial pressure (ICP) should be considered for all interventions. Drugs or alcohol, which may cause altered mental status and combative behavior, complicate the determination of the presence of closed head injury and the need for emergent airway management.
INDICATIONS FOR AIRWAY MANAGEMENT IN THE TRAUMA PATIENT
The most common reasons for deciding to perform endotracheal intubation (ETI) in the acutely injured patient are for oxygenation, ventilation, and airway protection. Severe chest and pulmonary injuries, hemorrhage, traumatic brain injury, and airway obstruction may lead to the inability of trauma patients to adequately oxygenate or ventilate. Protective airway reflexes may be impaired due to depressed mental status from traumatic brain injury, severe alcohol intoxication, and upper airway trauma. Trauma patients are often combative and resistant to calming techniques as well as physical and chemical restraints. These patients may benefit from intubation in these circumstances to expedite their evaluation. The increasing frequency of elderly trauma patients, who commonly have comorbidities, may provoke the clinician to consider early airway interventions to facilitate both the assessment and treatment of their traumatic injuries.
TECHNIQUES OF AIRWAY MANAGEMENT
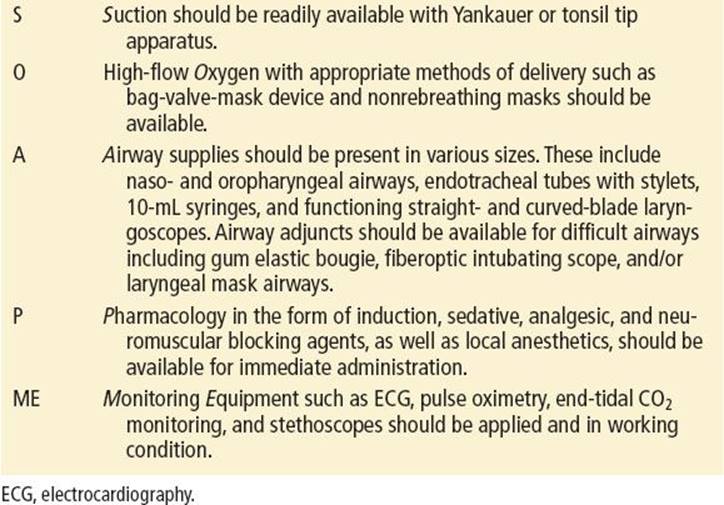
Orotracheal intubation (OTI), video-assisted intubation (VAI), blind nasotracheal intubation (NTI), and surgical cricothyrotomy are choices for definitive airway management in the trauma patient. Proper preparation is essential in the anticipation and execution of all airway interventions. The use of the mnemonic SOAPME may be helpful to ensure readiness (eTable 19.1).
eTABLE 19.1
Preparation for Airway Management: Mnemonic
Orotracheal Intubation and Rapid Sequence Induction
OTI may be performed in several ways, ranging from having the patient totally awake to performing OTI in conjunction with rapid sequence induction (RSI). OTI with RSI is the preferred approach to the airway management of the majority of patients with traumatic injuries. Although different pharmacologic agents may be chosen for neuromuscular blockade and induction, the major components of this intervention include preoxygenation, administration of agents that cause loss of consciousness (induction), administration of paralytics (neuromuscular blockade), and administration of postintubation analgesia and sedation.
Preoxygenation is performed to maintain hemoglobin saturation during airway management. Desaturations below 70% put patients at risk for dysrhythmia, hemodynamic decompensation, hypoxic brain injury, and death. Preoxygenation is achieved either actively or passively. A logistic flow of preoxygenation to prevent desaturation is shown in eFigure 19.1 (7).
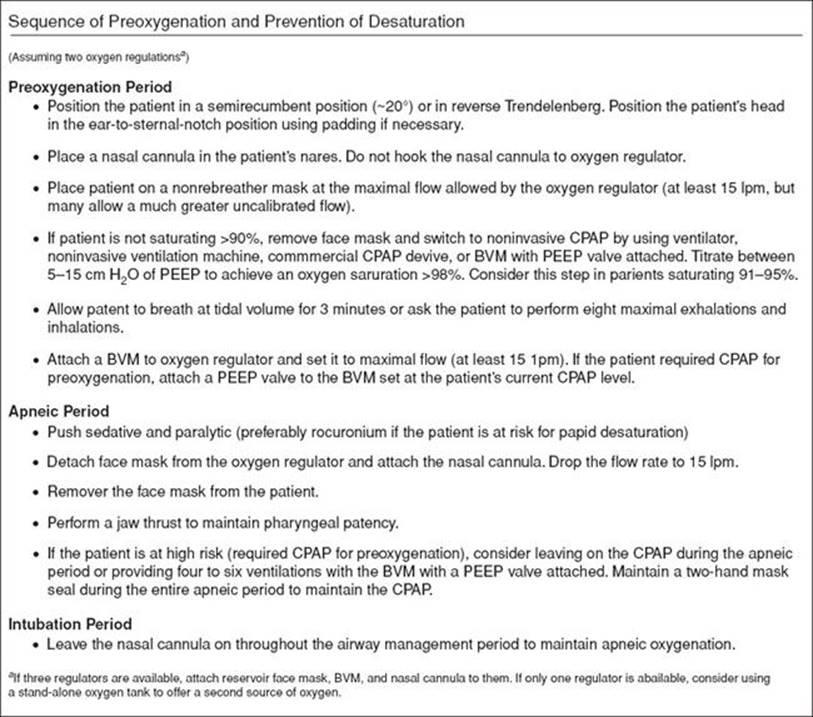
eFIGURE 19.1 Logistic flow of preoxygenation and prevention of desaturation. (From Weingart SD, Levitan MD. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59:165–175, with permission.)
A standard reservoir facemask with the oxygen flow rate set as high as possible is the recommended source of high FiO2 in the emergency department (ED). A passive approach will allow for spontaneous respirations through this nonrebreather facemask.
Active preoxygenation techniques should be considered for patients who cannot achieve greater than 95% oxygen saturation even with high FiO2 delivered passively. The risk categorization of patients during preoxygenation and the means by which oxygen should be applied is shown in eTable 19.2 (7). Active techniques for oxygenation include the use of continuous positive airway pressure (CPAP) masks, noninvasive positive-pressure ventilation, or positive end-expiratory pressure (PEEP) valves on a bag-valve mask (BVM). Optimal application of a BVM for the purposes of oxygenation and ventilation in the trauma patient typically requires two medical providers: one to ensure a proper mask-to-patient seal and one to manage bag compression.
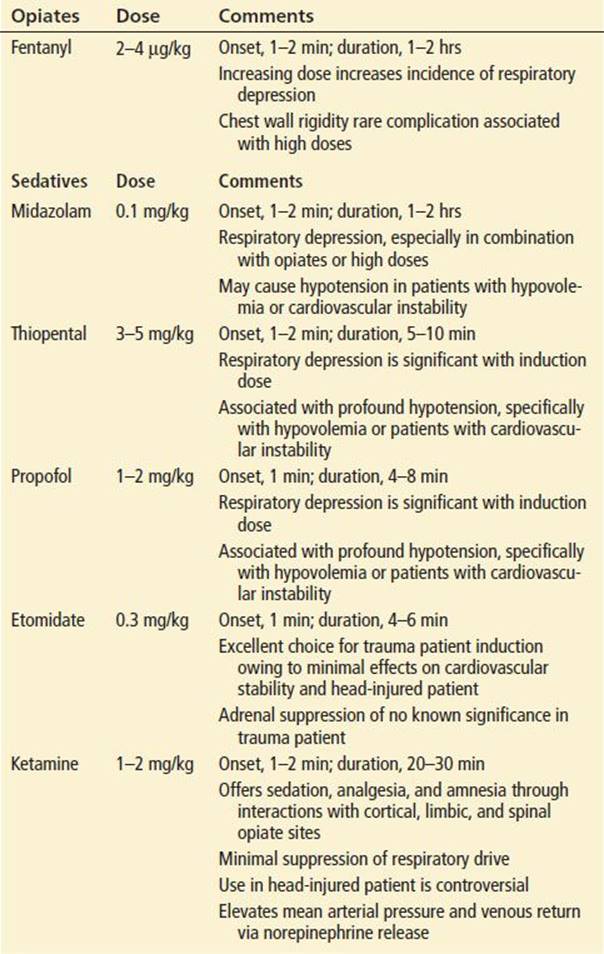
TABLE 19.2
Selected Pharmacologic Agents for Use During Trauma Airway Management
eTABLE 19.2
Risk Categorization of Patients During Preoxygenation
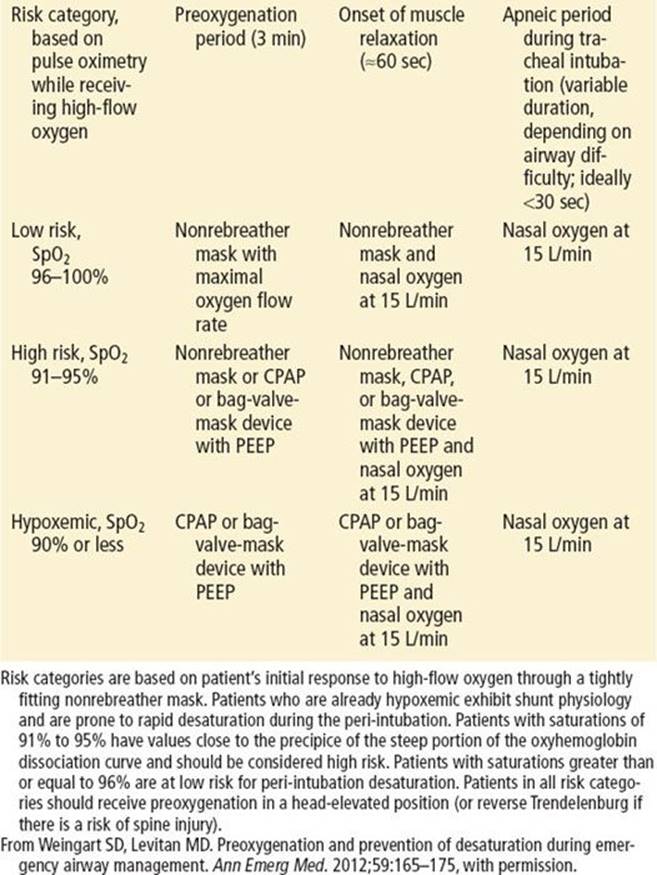
Apneic oxygenation is also a key component of adequate preoxygenation. When high flow oxygen (15 L/min) is delivered through a nasal cannula after induction and during the apneic period patients can maintain oxygen saturations of more than 98% for 18 to 55 minutes (5).
Difficulty in providing maximal preoxygenation may occur in patients with chest trauma or those with bronchospasm from pre-existing reactive airway disease or from smoke inhalation. In cases where pneumothorax is strongly suspected, consideration should be given to delaying intubation and mechanical ventilation until after performance of tube or needle thoracostomy. Artificial ventilation can result in rapid progression of a simple pneumothorax to a tension pneumothorax, even with a brief period of mechanical ventilation.
Neuromuscular blockade is performed during RSI for a number of reasons. Muscular paralysis reduces the aspiration risk by eliminating the gag and cough response to laryngoscopy. Paralysis also effectively relaxes the upper airway musculature to allow for an optimal view of the larynx. It prevents patient movements that might complicate efforts to visualize the airway during intubation. Caution should be exercised in the use of paralytic agents if difficulty ventilating the patient via BVM is anticipated.
Rescue airway adjuncts, as well as cricothyrotomy equipment, must be immediately available at all times during RSI of trauma patients. In cases where a difficult airway is anticipated, a modified approach may be used to provide adequate sedation or anesthesia to allow for airway intervention without the use of neuromuscular blocking agents.
Video-Assisted Intubation
Video-assisted devices are becoming more commonplace in EDs, particularly in the training environment. There have been many studies to date that have shown users obtain better laryngeal visualization and have a higher first-pass success rate in the difficult airway patient (6). There are many commercially available video laryngoscopes and all require some added training. Even in the hands of novice video laryngoscopy improves visualization and visual confirmation of proper tube placement (eFig. 19.2). Intubation can be performed by passing a tube over a flexible fiberoptic scope while visualizing the vocal cords or using a rigid video laryngoscope, such as the Glidescope or Storz video system. The same principles of RSI apply when using a video device.
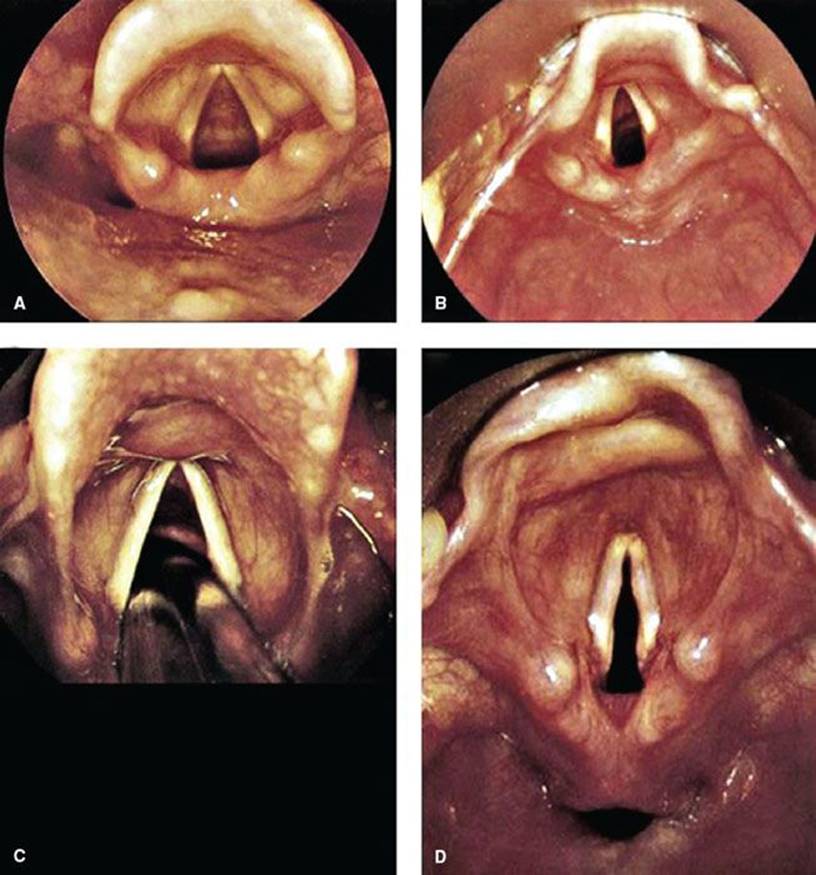
eFIGURE 19.2 Larynx appearance with videolaryngoscope. A: Preintubation view of an adult airway. B: Preintubation view of a pediatric airway. C: ETT passing between the vocal cords. D: The larynx and hypopharynx (note the horizontally oriented space below the laryngeal inlet, which is the esophagus). (From Nagdev A. Airway, breathing, circulation: Normal airway. In: Greenberg MI, Hendrickson RG, Silverberg M, et al., eds. Greenberg’s Text-atlas of Emergency Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 2004, with permission.)
The utility of the video-assisted device is limited in certain trauma situations particularly when visualization is impaired by blood, vomit, secretions, or direct trauma to the airway. As with any intubation attempt proper preparation should include having backup plans for failed attempts, this includes the ability to perform direct laryngoscopy and the tools for a surgical airway.
Blind Nasotracheal Intubation
NTI has several drawbacks and few advantages when compared to other techniques that are readily available for emergency airway management. Nasotracheal intubation requires a clinician who is experienced in the technique, a cooperative patient who is spontaneously breathing, and proper preparation of the nasal mucosa. This technique has largely fallen out of favor because it is more time consuming, has a larger failure rate, a higher complication rate, and requires a smaller tube size than other techniques. Despite these drawbacks NTI is still an important skill because it may be useful in certain situations such as limited mouth opening or severe oral trauma. The safety of NTI in patients with significant midface trauma has been suggested in clinical experience and the literature (13).
If NTI is attempted, oxygen should be administered by high-flow delivery throughout the procedure to improve oxygenation. The larger nostril should be chosen for placement of the endotracheal tube. The nasal mucosa should be prepared using a topical anesthetic and vasoconstrictive agent such as 4% lidocaine and 1% phenylephrine. Mild or moderate sedation may improve patient cooperation and decrease patient movement. Endotracheal tubes specifically designed for NTI are helpful as well, including tubes in which the tip can be manipulated anteriorly by a proximal trigger, thus enhancing the success of tracheal placement.
Surgical Airway Management
Cricothyrotomy equipment should be immediately available for any trauma patient undergoing emergent airway interventions, including RSI. The major indication for cricothyrotomy is failure of other methods of intubation with the simultaneous inability to ventilate and oxygenate the patient via BVM. Many cricothyrotomies involve patients with significant facial trauma or upper airway hemorrhage.
Patients with anterior neck trauma (penetrating and blunt) deserve particular consideration since they have a relative contraindication to cricothyrotomy. In addition, there will always be a small percentage of patients whose oral anatomy or body habitus renders intubation by any means very difficult and limits the feasibility of using airway adjuncts for more than a very limited amount of time. Perhaps the greatest mistake regarding the use of cricothyrotomy is its timing, as it is frequently used too late in the course of management when the patient is already severely hypoxemic.
Special Maneuvers and Intubation Adjuncts
Displacement of the thyroid cartilage Backward against the cervical vertebrae, Upward or as superiorly as possible, and laterally to the Right (the BURP maneuver) has been described and demonstrated to improve the view of the glottis during laryngoscopy (eFig. 19.3) (22). The mechanism by which BURP improves visibility may lie in the ability to move the glottis into the line of vision given that laryngoscopy tends to push the tongue and possibly the larynx toward the left. Application of the BURP maneuver may require a third provider in addition to the laryngoscopist and individual holding inline stabilization of the neck.
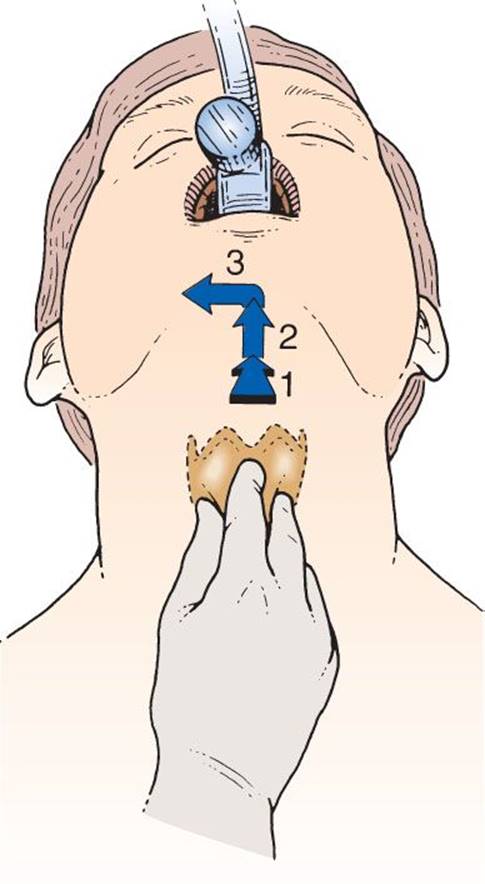
eFIGURE 19.3 Diagram of application of the BURP maneuver to improve the glottic view during laryngoscopy. The thyroid cartilage is moved Backward against the cervical vertebrae, Upward or as superiorly as possible, and laterally to the Right.
Several airway adjuncts can aid in the intubation process or are designed to temporarily substitute for intubation if it cannot be performed (3,14). These devices should be included as part of the difficulty airway algorithm for trauma airway management. The lighted stylet and gum elastic bougie, allow blind placement (placement without visualization of the vocal cords) of an endotracheal tube (12). Ventilation and oxygenation adjuncts for temporary airway support in the sedated or unconscious patient include the laryngeal mask airway (LMA), the combitube, and the King airway. LMAs are increasingly utilized as rescue airway devices for the failed intubation patient and often provide excellent airway management until intubation can be achieved. LMAs that allow for intubation through the lumen of the device have been developed and should be considered for their potential to achieve airway management as a blind intubation technique.
Pharmacologic Agents
Pharmacologic agents are chosen to accomplish several goals including topical anesthesia, sedation, analgesia, amnesia, and paralysis. Judicious use of these agents may facilitate intubation while avoiding such complications as increases in ICP and emesis. Selection of the proper agent in the trauma setting is essential to avoid complications such as prolonged paralysis with inability to ventilate, rises in ICP, or cardiovascular deterioration. There is very little published data from the acute care setting upon which to base and evidence-based practice for trauma airway management. As a result, preference for specific agents is based largely on theoretical principles as well as extrapolation of data from other settings. There is no pharmacologic agent that has been proven to offer a comprehensive advantage without limitations when compared to other selections.
Local Anesthetics
Lidocaine is an amide that can be used topically, locally, or intravenously to aid in airway management. Maximum doses are 3 to 4 mg/kg. When applied topically in a 4% solution, lidocaine may be used with topical vasoconstrictors to aid in NTI. Nebulization of a 4% solution to a spontaneously breathing patient can produce complete topical anesthesia of the oro- and nasopharynx and the vocal cords in 5 to 7 minutes (4). When given intravenously, in a dose of 1.5 to 2 mg/kg 2 to 3 minutes prior to intubation, lidocaine may attenuate the hemodynamic and cough reflex–mediated rise in ICP (20). This application remains controversial with debatable advantages and few drawbacks other than complicating the RSI approach by addition of another agent.
Induction Agents
Sedatives, hypnotics, and potent opioid analgesics may be used as pharmacologic adjuncts to achieve states ranging from light sedation to complete loss of consciousness (Table 19.2). There is a balance between the risks and potential benefits for each of these agents in the trauma setting. The hemodynamic effects of each agent should be a primary consideration. Additional considerations include the following factors: (a) the agent’s reliability of induction at a given dose, (b) the need to maintain spontaneous respiration, (c) the likelihood of a traumatic brain injury, and (d) the patient’s pre-existing physiologic state including comorbidities.
Although adverse effects on respiration can be countered in most instances with artificial ventilation, there is no simple maneuver to counteract the cardiac dysfunction that may be produced by these agents in the trauma victim.
Barbiturates
Thiopental and methohexital are very short-acting sedative, hypnotic agents with no analgesic properties. Their onset of action is within 1 minute with duration of clinical effects between 5 and 10 minutes (21). The benefits of these agents are their induction reliability and rapidity of onset.
The major disadvantage of barbiturates is their effect on cardiovascular stability in the hemodynamically compromised patient, primarily due to significant reductions in venous return and contractility (21). While these effects are typically not a major consideration in the nontrauma patient, their use in the hypovolemic or unstable trauma patient may result in sudden, profound hypotension as well as reduction in cerebral perfusion pressure. Given the principle that all acutely injured trauma patients should be assumed to have injuries rendering them unstable from a cardiovascular standpoint, the use of barbiturates in this population should be approached with caution. If barbiturates are to be utilized, meaningful reductions in induction dosages should be employed with thiopental doses ranging from 0.5 to 1 mg/kg are generally recommended (21).
Propofol
Propofol is a substituted isoprophylphenol that is highly lipophilic and capable of producing profound sedation, hypnosis, and amnesia, with no analgesic properties (21).
A unique characteristic of propofol is its rapid metabolic clearance and redistribution, which is approximately 10 times faster than thiopental. Clinical recovery is rapid, occurring within 4 to 8 minutes, with little residual sedation.
Caution must be exercised if propofol is used in the undifferentiated trauma patient, particularly owing to the hemodynamic effects on venous return that often result in clinically observed decreases in blood pressure. Propofol should be avoided in patients at high risk for hemodynamic compromise and instability due to hemorrhage or hypovolemia.
The primary use of propofol in the trauma setting is as a postintubation sedative with continuous infusion. The brief duration of clinical effects associated with propofol allows for rapid recovery of neurologic status and levels of consciousness. This advantage is often cited as a benefit in the trauma patient who may undergo recurrent neurologic assessments over an extended time period.
Etomidate
Etomidate is a carboxylated imidazole induction agent with no analgesic properties (21). In doses of 0.3 mg/kg, induction is reliably produced in <1 minute, and the duration of action is between 6 and 8 minutes. Etomidate has several properties that make it attractive for use in the multisystem trauma patient. When given in single induction boluses, etomidate causes minimal changes in heart rate and cardiac output compared with equipotent doses of thiopental (21). This is particularly advantageous in patients with hypotension or compensated shock, as well as in those with pre-existing myocardial dysfunction.
Etomidate also causes significantly less respiratory depression than barbiturate agents, although transient apnea may occur when it is given rapidly. Etomidate may in fact stimulate ventilation. For this reason it may be advantageous when maintenance of respiration is desirable, such as during sedation with NTI or modified RSI.
Although etomidate occasionally causes side effects, there are no contraindications to its use as a single injection in the trauma patient. Side effects include transient burning on injection, transient myoclonus after administration in up to 40% of patients, and transient suppression of endogenous cortisol production for up to 12 hours after single bolus administration. The temporary suppression of cortisol production has not been demonstrated to affect outcome in the trauma patient and should not limit the use of etomidate in this population (15,21).
Ketamine
Ketamine is a phencyclidine derivative that produces dissociative anesthesia. It is the only agent commonly used for induction in the ED that possesses sedative, hypnotic, analgesic, and amnestic properties (21). Ketamine provides the most cardiovascular and respiratory support of any agent. Although it is a direct myocardial depressant, heart rate and blood pressure are usually maintained or increased owing to centrally mediated sympathetic stimulation via increases in norepinephrine. Central sympathetic stimulation also results in transient bronchodilation.
The major advantage of ketamine, in comparison to other agents, lies in the setting of the hypovolemic patient (21). Its onset of action is within 1 minute when given intravenously (1 to 2 mg/kg), with a duration of action ranging from 5 to 15 minutes. Ketamine may also be given intramuscularly (4 mg/kg), with the onset of action delayed by several minutes.
Because it is a phencyclidine derivative, ketamine can cause an emergence delirium. Though this is a concern during procedural sedation, it should not prohibit its use as an intubation adjunct in a critically ill trauma patient. Intubated trauma patients are typically kept sedated and paralyzed for many hours after their initial presentation, and emergence delirium at that time is rare (21). Continued sedation with benzodiazepines virtually eliminates this issue as a concern.
The primary concern with the use of ketamine in the trauma population is its potential to affect ICP owing to its ability to increase cerebral blood flow by 30% to 60% (21). Even though the cerebral metabolic rate is increased with ketamine, cerebral blood flow is probably sufficient to meet demand. There is evidence that this increase in cerebral blood flow does not increase ICP (11). In fact, there is evidence that ketamine is neuroprotective in the setting of head trauma because it is an N-methyl-D-aspartate receptor antagonist (19). The use of ketamine may be warranted in the setting of head injury when induction is required in a hypotensive patient. Any reduction in MAP has greater potential to worsen cerebral ischemia than to affect clinical outcome from a transient rise in ICP.
The routine use of ketamine in the trauma patient remains an area of controversy. Its use in the hypotensive patient appears to be a reasonable decision given the relative concerns for other agents in this setting.
Benzodiazepines
Benzodiazepines (diazepam and midazolam) have been used alone, and in combination with opioids, as induction agents. They provide good anxiolysis and amnesia, but no analgesia is provided. Large doses are usually needed to produce predictable states of induction equivalent to those of the agents discussed above (21). Midazolam is currently the most commonly used benzodiazepine for airway management. An induction dose of midazolam (0.1 mg/kg) takes effect within 1 to 2 minutes and has a duration of action between 30 and 60 minutes. Even at doses of 0.1 mg/kg, induction is not always predictable.
Benzodiazepines can be accompanied by side effects such as severe respiratory depression. Significant decreases in venous return, MAP, and cardiac contractility can also occur, especially in patients with hypovolemia or heart disease (1). All of these effects are more pronounced when opioids are given simultaneously.
Subinduction doses (0.03 to 0.05 mg/kg) of midazolam are not commonly associated with these complications and can serve as valuable adjuncts in providing continued sedation for patients after intubation.
Opiates
Synthetic opioid agonists including fentanyl, sufentanil, and alfentanil are 100, 500 to 1,000, and 20 times more potent than morphine, respectively (21). These agents are fast acting, having an onset of action of <1 minute, with a duration of action between 15 and 60 minutes.
Fentanyl results in little or no histamine release, and its cardiovascular effects in the normal host are minimal. At higher doses, however, small but potentially significant decreases in blood pressure may occur (21). Depending on the existing state of consciousness and the presence of drugs such as alcohol, the dose necessary to produce unconsciousness can range from 2 to 20 μg/kg or more. The effect of fentanyl on ventilation varies, but doses >2 μg/kg result in a high incidence of respiratory depression in “normal” subjects (2). This incidence is even higher when used together with other agents such as midazolam.
Fentanyl is often used as a preinduction adjunct for intubation of the head-injured patient owing to its ability to attenuate the hemodynamic response to intubation. However, when given in doses sufficient to achieve this effect, 2 to 3 μg/kg given 2 to 3 minutes before laryngoscopy, increases in ICP may occur that may negate any advantage to its use in the setting of traumatic brain injury. Decreases in MAP were also noted to occur after administration of fentanyl at these doses. Coupled with the potential for producing premature hypoventilation and apnea, this makes the routine use of these agents as induction or preinduction agents in the setting of multisystem trauma controversial. An additional role for these opiates is to provide postintubation sedation and analgesia to attenuate the hyperdynamic responses from pain and intubation and for patient comfort.
In summary, despite the most careful use of pharmacologic agents, any induction agent may result in sudden and profound hypotension unresponsive to simple fluid boluses. In cases of head injury, hypotension, even if transient, can result in prolonged cerebral hypoperfusion (16).
Neuromuscular Blocking Agents
The use of neuromuscular blocking agents to facilitate intubation has become widespread in emergency airway management. These agents are classified as depolarizing and nondepolarizing agents.
Depolarizing Agents
Succinylcholine (1.5 to 2.0 mg/kg) is the agent of choice during emergent RSI. No neuromuscular blocking agent has a faster onset (<1 minute) or is of shorter duration (4 to 6 minutes). Succinylcholine can also be given intramuscularly (4 mg/kg), but its onset is delayed by 2 to 4 minutes.
The disadvantages of succinylcholine in the trauma patient population are relatively few and should not preclude its use in the acutely injured patient. Fasciculations, hyperkalemia, and transient rises in intragastric, intraocular, and ICP may occur (9). Succinylcholine-induced hyperkalemia in burns and crush injuries does not occur in the acute setting. If fasciculations and elevated intraocular, intragastric, and ICP are major concerns, administration of a defasciculating dose of a nondepolarizing agent (i.e., vecuronium 0.01 mg/kg) 2 to 3 minutes before succinylcholine administration has been demonstrated to prevent these occurrences (21). If a defasciculating dose of a nondepolarizing agent is used, the dose of succinylcholine should be increased to 1.5 to 2 mg/kg to maintain its rapidity of onset.
Nondepolarizing Agents
There are several nondepolarizing neuromuscular blocking agents in current use. Vecuronium and rocuronium are the major nondepolarizing agents used in trauma airway management. The advantages of these agents are that they are longer acting, cause no fasciculations, and cause no reported increase in intraocular, intragastric, or ICP. These agents also have little effect on the cardiovascular system (9,21).
The standard dose of vecuronium for paralysis is 0.15 mg/kg. This results in complete paralysis within 2 to 3 minutes, with a duration of action of 30 to 40 minutes. The onset of action of rocuronium (0.9 mg/kg) approaches that of succinylcholine, although its duration of action is similar to that of vecuronium (25 to 40 minutes) (21).
A major disadvantage of vecuronium and rocuronium in the trauma patient is the relatively slower onset of clinical effects, taking up to 2 to 3 minutes for a full clinical effect. Large doses of vecuronium (0.25 mg/kg) and rocuronium (1.2 mg/kg) may be used as an initial bolus to achieve more rapid paralysis within 60 to 90 seconds. However, this strategy lends an extended period of duration of paralysis, lasting as long as 90 minutes. The duration of action of nondepolarizing agents is longer relative to succinylcholine, creating significant problems if intubation attempts are unsuccessful.
Nondepolarizing agents can be reversed to some extent by drugs that block cholinesterases, such as neostigmine, edrophonium, and pyridostigmine. The routine use of these reversal agents in the acutely injured patient is not advised owing to the potential for cardiovascular complications.
SPECIAL CONSIDERATIONS
Cervical Spine Injury
OTI utilizing RSI is now the preferred procedure to achieve definitive airway control in patients with suspected cervical injury (17). As positioning the airway in this setting is limited, use of a straight laryngoscope blade may be preferable to a curved blade because it will lift the epiglottis directly. The use of VAI has also been shown to be of particular benefit in these patients with an improved first-pass success rate (6).
Removal of the front of the cervical collar while maintaining in-line immobilization (not traction) significantly improves the view of the larynx during intubation and should be a routine component in airway management of the trauma patient (8). When manual immobilization is being performed, an applied cervical collar offers no significant advantage.
Regardless of approach, airway management in the setting of potential cervical spine injury is optimally performed with at least three people: one as the laryngoscopist, one to provide in-line immobilization of the cervical spine, and one to perform cricoid pressure. Rational use of airway adjuncts such as special laryngoscopes, the gum elastic bougie, and the LMA may be indicated based on the experience of the operator.
Penetrating Neck Trauma
In cases of penetrating neck trauma with possible altered upper airway anatomy or signs of airway obstruction, OTI with RSI is the procedure of choice when injuries do not impair OTI visualization (18). Administration of paralytics may be strategically deleted if proper sedation and upper airway anesthesia are provided.
Use of induction agents with less effect on ventilation (etomidate and ketamine), along with intravenous or nebulized lidocaine, will aid in reduction of gagging and further hemorrhage and anatomic distortion of the neck. Ketamine without paralysis is an alternative as it preserves respiratory drive. This may be essential for intubating patients who have anatomic distortion owing to an expanding hematoma. The presence of anterior neck trauma is a relative contraindication to cricothyrotomy.
Head Injury
The pathophysiology of traumatic brain injury is complex and involves a combination of mechanical and biochemical events initiated by the trauma itself, followed by secondary injury in the form of ischemia. The most preventable forms of secondary brain injury are systemic hypoxemia and hypotension. Because most head injuries occur in association with multisystem trauma, a reasonable approach would be to administer agents that cause a predictable loss of consciousness, cause no increase in ICP, and maximize the chance to maintain MAP.
Traditional approaches to the head trauma victim requiring intubation assumed that the brain had lost some degree of its ability to autoregulate its blood flow. The MAP minus the ICP determines cerebral perfusion pressure and hence cerebral blood flow in this setting. Emphasis has been placed on blocking the rise in ICP during intubation with the use of agents such as barbiturates. However, maintaining the mean arterial pressure in these circumstances is critical given that cerebral blood flow is directly related to perfusion.
Although an attempt to block the rise in ICP during intubation of the head-injured patient is of theoretical benefit, this concern has not been demonstrated to affect outcome in controlled studies. Attempts to manage ICP during intubation must be carefully balanced with the pharmacologic agent’s effect on blood pressure, as lowering mean arterial blood pressure may lower cerebral blood flow and cause secondary ischemic brain injury (16).
Facial Trauma
Patients with facial injuries represent an airway management challenge, especially when there is severe upper airway hemorrhage. The airway management technique of choice depends on several factors, including the patient’s level of consciousness, level of oxygenation, amount of upper airway hemorrhage, and risk of other injuries such as cervical spine injury. The availability of one or more large-volume suctioning devices is critical if upper airway hemorrhaging is present. OTI with RSI remains the best approach in the majority of facial trauma cases.
Airway adjuncts should be readily available in all trauma patient encounters, particularly in those patients with facial injuries. If OTI is unsuccessful, placement of the esophageal tracheal combitube or LMA can reverse hypoxemia and temporarily protect the airway while cricothyrotomy is performed. Fiberoptic laryngoscopy may be of limited use in these patients as blood and other secretions render visualization of the glottis a challenge.
SUGGESTED APPROACHES
In most emergent trauma airway management scenarios, OTI with RSI using in-line cervical stabilization is the preferred approach. This approach should be followed with continued sedation and analgesia. The immediate concerns in this population are the prevention of hypoxemia and hypotension.
• The physician should assume that every trauma patient is hypovolemic, even if there are no signs of shock during the initial evaluation.
• The clinician should assume that all victims of blunt trauma have suffered an intracranial injury, with loss of cerebral blood flow autoregulation.
• All patients should be treated as if a cervical spine injury is present.
• The patient should not experience further decreases in MAP secondary to administration of medications or airway maneuvers.
• The patient should not develop premature apnea or hypoventilation.
• The patient should not develop large increases in ICP.
Figure 19.1 outlines intubation algorithms that will meet the needs of the majority of severely injured trauma patients.
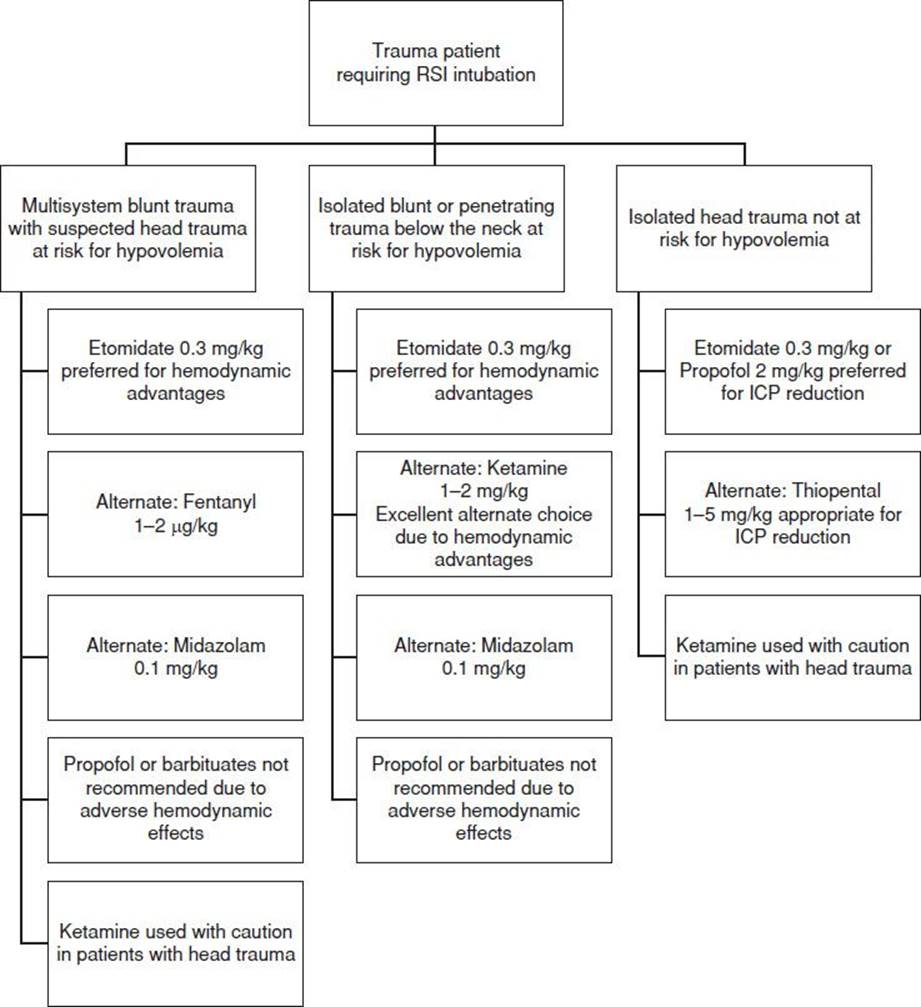
FIGURE 19.1 Algorithm for selection of induction agent in trauma airway management with preferred induction agent and alternate choices.
After intubation, small, frequent doses of midazolam (1 to 3 mg) and fentanyl (50 to 100 μg) are appropriate for sedation and are not typically associated with major side effects. Longer-acting agents such as lorazepam and morphine may also be used.
Once significant hemorrhage or hemodynamic instability has been ruled out, more easily titrated agents such as propofol can be used in a continuous infusion for sedation. Continued paralysis while simultaneously providing analgesia and sedation, may be required to optimize resuscitation and diagnostic workup. Early removal of patients from spine immobilization boards, proper splinting of fractures, and application of local anesthetics to wounds significantly decrease the patient’s discomfort.
Common Pitfalls
• Failure to consider occult hypovolemia, shock, and pre-existing disease states when choosing induction agents.
• Failure to maintain cervical spine stabilization during intubation in patients with suspected cervical spine injuries.
• Failure to have airway rescue adjuncts available for difficult airway situations.
• Failure to have a preplanned and prepared sequence of alternative airway approaches in case of failure of initial intubation attempts.
• Failure to provide adequate ongoing postintubation sedation and analgesia.
REFERENCES
1. Adams P, Gelman S, Reves JG, et al. Midazolam pharmacodynamics and pharmacokinetics during acute hypovolemia. Anesthesiology. 1985;63:140–146.
2. Bailey PL, Pace NL, Ashburn MA, et al. Frequent hypoxemia and apnea after sedation with midazolam and fentanyl. Anesthesiology. 1990;73:826–830.
3. Blostein PA, Koestner AJ, Hoak S. Failed rapid sequence intubation in trauma patients: Esophageal tracheal combitube is a useful adjunct. J Trauma. 1998;44: 534–537.
4. Bourke DL, Katz J, Tonneson A. Nebulized anesthesia for awake endotracheal intubation. Anesthesiology. 1985;63:690–692.
5. Nemeth J, Maghraby N, Kazim S. Emergency airway management: The difficulty airway. Emerg Med Clin North Am. 2012;30:401–420.
6. Aziz M. Use of video-assisted intubation devices in the management of patients with trauma. Anesthesiology Clin. 2013;31:157–166.
7. Weingart SD, Levitan MD. Preoxygenation and prevention of desaturation during emergency airway management. Ann Emerg Med. 2012;59:165–175.
8. Heath KJ. The effect of laryngoscopy of different cervical spine immobilization techniques. Anaesthesia. 1994;49:843–845.
9. Hunter JM. New neuromuscular blocking drugs. N Engl J Med. 1995;332:1691–1699.
10. Kaups KL, Davis JW. Patients with gunshot wounds to the head do not require cervical spine immobilization and evaluation. J Trauma. 1998;44:865–867.
11. Mayberg TS, Lam AM, Matta BF, et al. Ketamine does not increase cerebral blood flow velocity or intracranial pressure during isoflurane/nitrous oxide anesthesia in patients undergoing craniotomy. Anesth Analg. 1995;81:84–89.
12. Nolan JP, Wilson ME. Orotracheal intubation in patients with potential cervical spine injuries. An indication for the gum elastic bougie. Anaesthesia. 1993;48: 630–633.
13. Rosen CL, Wolfe RE, Chew SE, et al. Blind nasotracheal intubation in the presence of facial trauma. J Emerg Med. 1997;15:141–145.
14. Rosenblatt WH, Murphy M. The intubating laryngeal mask: Use of a new ventilating-intubating device in the emergency department. Ann Emerg Med. 1999;33:234–238.
15. Schenarts CL, Burton JH, Riker RR. Adrenocortical dysfunction following etomidate induction in emergency department patients. Acad Emerg Med. 2001;8: 1–7.
16. Schmoker JD, Zhuang J, Shackford SR. Hemorrhagic hypotension after brain injury causes an early and sustained reduction in cerebral oxygen delivery despite normalization of systemic oxygen delivery. J Trauma. 1992;32:714–720.
17. Shatney CH, Brunner RD, Nguyen TQ. The safety of orotracheal intubation in patients with unstable cervical spine fracture or high spinal cord injury. Am J Surg. 1995;170:676–679.
18. Shearer VE, Giesecke AH. Airway management for patients with penetrating neck trauma: A retrospective study. Anesth Analg. 1993;77:1135–1138.
19. Smith DH, Okiyama K, Gennarelli TA, et al. Magnesium and ketamine attenuate cognitive dysfunction following experimental brain injury. Neurosci Lett. 1993;157:211–214.
20. Splinter WM, Cervenko F. Haemodynamic responses to laryngoscopy and tracheal intubation in geriatric patients: Effects of fentanyl, lidocaine and thiopentone. Can J Anaesth. 1989;36:370–376.
21. Stoelting RK. Barbiturates. In: Stoelting RK, ed. Pharmacology and Anesthesiology in Anesthetic Practice. 2nd ed. Philadelphia, PA: JB Lippincott; 1991:70–172.
22. Takahata O, Kubota M, Mamiya K, et al. The efficacy of the “BURP” maneuver during a difficult laryngoscopy. Anesth Analg. 1997;84:419–421.